Hiring a skilled pharmacy technician is more than just finding someone who can count pills; it's about entrusting a professional with patient safety and regulatory compliance. The interview process can be tricky, as it requires a approach that tests not only knowledge but also their attention to detail and customer service abilities. Explore our insights on importance of attention to detail in the workplace.
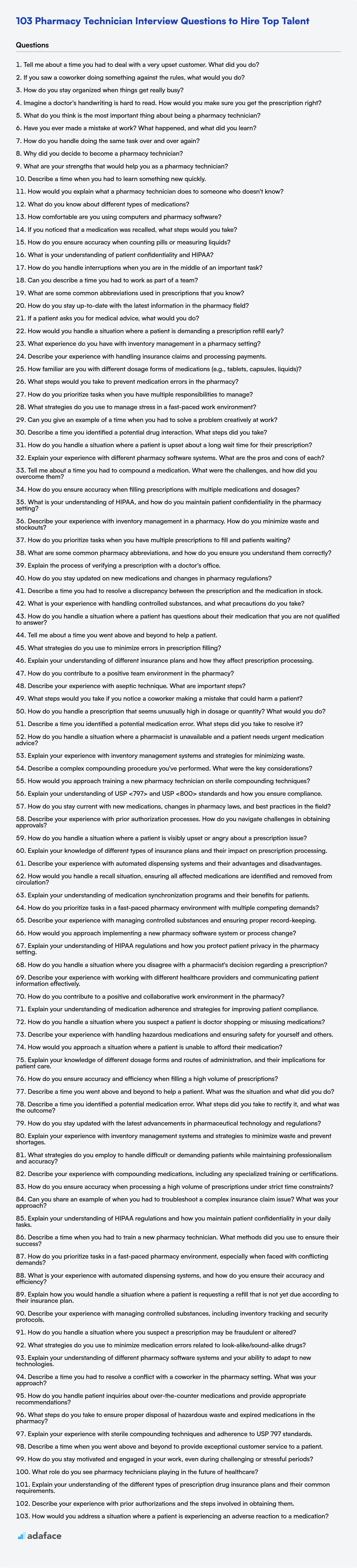
This blog post provides a treasure trove of interview questions, categorized by skill level, to help you identify the ideal candidate. From basic knowledge to expert insights, we've compiled a list covering a spectrum of topics, as well as a bonus section with multiple-choice questions.
By using these questions, you'll enhance your ability to assess candidates thoroughly, ensuring you hire a pharmacy technician who excels in both technical skills and patient care, and to make your recruitment process more , use the Pharmacy Technician Test before the interviews.
Table of contents
Basic Pharmacy Technician interview questions
1. Tell me about a time you had to deal with a very upset customer. What did you do?
I recall a situation where a customer was extremely frustrated because their order was delayed significantly beyond the promised delivery date. The first thing I did was actively listen and acknowledge their anger without interruption, letting them vent their frustrations. I then apologized sincerely for the inconvenience caused and took ownership of the problem even though it wasn't directly my fault.
Next, I investigated the reason for the delay and provided the customer with a transparent explanation. I also offered a concrete solution – in this case, expediting the delivery and offering a partial refund for the inconvenience. I made sure to follow up proactively to ensure the issue was resolved to their satisfaction and that they received their order. By actively listening, showing empathy, taking ownership, and providing a solution, I was able to de-escalate the situation and turn a negative experience into a positive one.
2. If you saw a coworker doing something against the rules, what would you do?
My response would depend on the severity and nature of the rule violation. If it's a minor infraction, I might first speak directly and privately with my coworker to understand the situation and gently remind them of the rule. This allows for a chance to correct the behavior without escalation.
However, if the violation is serious, such as involving safety, ethical concerns, or company policy with significant implications, I would report it to the appropriate authority, such as my manager, HR, or a compliance officer. I believe it's important to prioritize the integrity of the workplace and the well-being of the company and its employees, even if it means having a difficult conversation or reporting a colleague.
3. How do you stay organized when things get really busy?
When things get really busy, I rely on a few key strategies to stay organized. First, I prioritize tasks using a system like the Eisenhower Matrix (urgent/important) to focus on what truly matters. I create a detailed to-do list each day, breaking down large tasks into smaller, manageable steps. I use digital tools like a calendar and task management apps to schedule deadlines, set reminders, and track progress.
Second, I minimize distractions by setting specific times for checking email and social media. I block out time for focused work and communicate my availability to others. I also delegate tasks when possible and don't hesitate to ask for help when I'm feeling overwhelmed. Finally, I make sure to take short breaks throughout the day to recharge and avoid burnout. Consistently following these practices helps me to navigate busy periods effectively.
4. Imagine a doctor's handwriting is hard to read. How would you make sure you get the prescription right?
First, I would attempt to clarify the handwriting by consulting resources like online medical abbreviation databases or contacting a pharmacist, as they are trained to interpret prescriptions. If those options fail, I would prioritize patient safety above all else and directly contact the prescribing doctor's office or the doctor themselves to confirm the medication name, dosage, frequency, and route of administration before dispensing any medication. This ensures accuracy and prevents potential harm to the patient.
5. What do you think is the most important thing about being a pharmacy technician?
The most important thing about being a pharmacy technician is accuracy. Ensuring the correct medication, dosage, and instructions are provided to the patient is crucial for their health and safety. Mistakes can have serious consequences, so meticulous attention to detail is paramount.
Beyond accuracy, strong communication skills are also essential. Pharmacy technicians interact with pharmacists, patients, and other healthcare professionals. Clearly conveying information, actively listening to patient concerns, and maintaining a professional demeanor contribute significantly to the overall quality of patient care and helps create a positive pharmacy environment.
6. Have you ever made a mistake at work? What happened, and what did you learn?
Yes, I once deployed a code update to production that contained a bug causing intermittent errors for users. During a late-night release, I missed a critical integration test failure related to a specific edge case. As a result, a subset of users experienced issues accessing certain features. We quickly identified the root cause through monitoring and logs, and I worked with the team to roll back the deployment and implement a fix.
I learned the importance of thoroughly reviewing all test results, even when under pressure to meet deadlines. This experience reinforced the need for robust monitoring and automated rollback procedures. I've since become a strong advocate for incorporating more comprehensive testing and code review practices into our development workflow, especially when integrating new features or libraries.
7. How do you handle doing the same task over and over again?
When faced with repetitive tasks, I first assess if automation is possible. This could involve scripting (e.g., Python for file processing), using built-in tools, or exploring dedicated automation software. Automation reduces errors, saves time, and frees me to focus on more complex problems.
If automation isn't feasible, I focus on optimizing the process. This might involve breaking the task into smaller, more manageable steps, creating checklists to ensure consistency, or finding ways to improve my efficiency. I also ensure I have a clear understanding of the purpose of the task, which helps me stay motivated and identify potential improvements.
8. Why did you decide to become a pharmacy technician?
I was drawn to the pharmacy technician role because I wanted a career in healthcare where I could directly contribute to patient well-being and work in a fast-paced, detail-oriented environment. I am very interested in medication and the science behind them, and becoming a pharmacy technician provides a great opportunity to learn more about pharmacology.
Specifically, I was attracted to the combination of technical skills (like dispensing medication) and customer service. I enjoy helping people and believe I have the necessary skills to be a helpful and reassuring presence for patients when they come to pick up their prescriptions. I see it as a fulfilling career path where I can make a real difference in people's lives.
9. What are your strengths that would help you as a pharmacy technician?
My strengths align well with the demands of a pharmacy technician role. I possess strong attention to detail, which is crucial for accurately dispensing medications and preventing errors. I'm also highly organized, enabling me to manage inventory effectively and maintain a tidy workspace. Furthermore, I have excellent communication skills, allowing me to interact clearly and empathetically with patients and collaborate effectively with pharmacists and other healthcare professionals.
Beyond these core skills, I am a quick learner and adaptable to new procedures and software systems. I am also committed to maintaining patient confidentiality and adhering to all relevant regulations and ethical guidelines. My ability to prioritize tasks and remain calm under pressure would be valuable in a busy pharmacy environment.
10. Describe a time when you had to learn something new quickly.
During a project where we were migrating a legacy application to a new cloud platform, I needed to quickly learn Terraform. I had some basic understanding of Infrastructure as Code, but no practical experience with Terraform specifically.
To get up to speed, I started with the official Terraform documentation and tutorials. I also found a few online courses that provided hands-on examples. I then started experimenting in a development environment, creating simple infrastructure components and gradually increasing the complexity. I frequently consulted with more experienced colleagues and utilized online forums to troubleshoot issues. Within a week, I was able to contribute meaningfully to the project, automating the deployment of virtual machines, networks, and databases using Terraform. I focused on learning by doing and asking clarifying questions whenever necessary.
11. How would you explain what a pharmacy technician does to someone who doesn't know?
A pharmacy technician helps pharmacists dispense prescription medications to patients. They work under the supervision of a pharmacist and perform tasks such as:
- Measuring and preparing medications
- Counting pills and labeling bottles
- Entering prescription information into the computer
- Dealing with insurance companies for processing claims
- Handling money and managing inventory
- Answering phone calls and helping customers at the counter.
Essentially, they are the pharmacist's right-hand, assisting with all the behind-the-scenes tasks to ensure patients receive their medications safely and efficiently, which allows the pharmacist to focus on counseling patients and ensuring medication appropriateness.
12. What do you know about different types of medications?
Medications can be broadly categorized by how they work and what they treat. Common types include: analgesics (pain relievers like ibuprofen and acetaminophen), antibiotics (fight bacterial infections like penicillin and amoxicillin), antidepressants (treat depression, such as SSRIs like sertraline), anti-inflammatories (reduce inflammation, examples being corticosteroids and NSAIDs), and antihistamines (combat allergy symptoms, like diphenhydramine and loratadine).
Furthermore, medications can be classified by their route of administration (oral, topical, intravenous), their chemical structure (e.g., statins), or their therapeutic use (e.g., antihypertensives for high blood pressure). Understanding these categories is crucial for healthcare professionals to choose the appropriate treatment for a patient.
13. How comfortable are you using computers and pharmacy software?
I am very comfortable using computers and pharmacy software. I have several years of experience working with various operating systems (Windows, macOS), and I'm proficient with common office software (Microsoft Office, Google Workspace).
Regarding pharmacy software, I have hands-on experience with [mention specific software like Rx30, PioneerRx, or similar based on your actual experience]. I'm comfortable with tasks such as prescription processing, inventory management, insurance billing, and patient profile management. I am a quick learner and adapt easily to new software systems. I am familiar with HIPAA regulations and maintain patient confidentiality when working with sensitive data.
14. If you noticed that a medication was recalled, what steps would you take?
First, I would immediately verify the recall information through official sources like the FDA website or the manufacturer's website. This ensures the recall is legitimate and determines the scope of the recall (specific lot numbers, expiration dates, etc.).
Next, I would immediately stop dispensing or administering the recalled medication. If patients have already received the medication, I would follow established protocols to notify them about the recall, explain the potential risks, and advise them on what actions to take (e.g., return the medication, contact their doctor). I'd also document all actions taken and report the recall to the appropriate regulatory bodies.
15. How do you ensure accuracy when counting pills or measuring liquids?
To ensure accuracy when counting pills, I would use a pill counting tray or an automated pill counter if available. I would double-count the pills to verify the initial count. If counting by hand, I would organize the pills in rows for easier tracking. For measuring liquids, I'd use a graduated cylinder or a calibrated beaker appropriate for the volume being measured. The measurement would be taken at eye level, ensuring the meniscus is correctly aligned with the graduation mark. I'd also double-check the measuring device to ensure it is clean and free of any residue that could affect the reading.
16. What is your understanding of patient confidentiality and HIPAA?
Patient confidentiality is the ethical obligation to protect patient information. It means healthcare professionals must not disclose a patient's personal or medical details without their explicit consent. HIPAA (Health Insurance Portability and Accountability Act) is a US law that sets national standards to protect individuals' medical records and other personal health information. It establishes rules for who can access, use, and share a patient's protected health information (PHI). This covers things like medical history, test results, insurance information, and even conversations with healthcare providers.
17. How do you handle interruptions when you are in the middle of an important task?
When interrupted during an important task, I first politely acknowledge the interruption. I then quickly assess the urgency of the interruption. If it's genuinely urgent (e.g., a critical production issue), I'll address it immediately. Otherwise, I explain that I'm in the middle of something important and propose a specific time to discuss it later. For example, "I'm currently focused on completing this critical report. Can we talk about this at [specific time], or would it be better if I loop you in on the next meeting about it?"
Before switching to the interruption (if necessary), I make a quick note of where I am in my current task. This might involve writing down the next steps or saving any work in progress. This helps me quickly resume the original task later and minimizes context switching costs. I also find that keeping a running to-do list, categorized by priority, helps me stay focused and manage incoming requests effectively.
18. Can you describe a time you had to work as part of a team?
In a recent project, I collaborated with a team of four developers to build a REST API for a new e-commerce platform. My primary responsibility was to design and implement the user authentication and authorization modules. This required close coordination with the front-end developers to ensure seamless integration and a consistent user experience. We used daily stand-up meetings to discuss progress, identify roadblocks, and coordinate tasks.
Specifically, there was a point where we were facing performance issues with our database queries. I worked together with a database specialist in our team, and we profiled the queries. After some analysis, we identified a few slow queries that were missing indexes. We addressed them by adding composite indexes to the tables. We then used EXPLAIN ANALYZE to examine the query plans. This resulted in significant improvement of the API response times, and we successfully delivered the project on time. Furthermore, we documented our findings and created a guide for writing performant queries.
19. What are some common abbreviations used in prescriptions that you know?
Common abbreviations in prescriptions include: QD (quaque die, once a day), BID (bis in die, twice a day), TID (ter in die, three times a day), QID (quater in die, four times a day), PRN (pro re nata, as needed), PO (per os, by mouth), IM (intramuscular), IV (intravenous), SC (subcutaneous), STAT (statim, immediately), HS (hora somni, at bedtime), AC (ante cibum, before meals), PC (post cibum, after meals), OD (oculus dexter, right eye), OS (oculus sinister, left eye), OU (oculus uterque, both eyes), AU (auris utraque, both ears), AS (auris sinistra, left ear), AD (auris dextra, right ear), q (every), q.h. (every hour), q.d. (every day), Sig. (signetur, write on label), Rx (prescription), and Disp. (dispense).
20. How do you stay up-to-date with the latest information in the pharmacy field?
I stay current in the pharmacy field through a multi-faceted approach. I regularly read professional journals like the Journal of the American Pharmacists Association and Pharmacy Times. I also subscribe to email newsletters from organizations such as the ASHP and state pharmacy associations, which provide updates on new medications, regulations, and best practices.
Furthermore, I actively participate in continuing education (CE) programs, both online and in-person, focusing on areas relevant to my practice or areas where I want to expand my knowledge. Attending conferences and workshops offered by pharmacy organizations is another valuable way I learn about the latest advancements and network with other professionals in the field.
21. If a patient asks you for medical advice, what would you do?
As a large language model, I am not qualified to give medical advice. Providing medical guidance requires the expertise of a trained healthcare professional who can assess the patient's specific situation, medical history, and perform necessary examinations.
I would advise the patient to consult with a qualified doctor, nurse, or other healthcare provider. I can, however, help them find resources such as locating nearby medical facilities or providing general information from reliable medical websites like the Mayo Clinic or the National Institutes of Health. It is crucial to always prioritize professional medical consultation for health concerns.
22. How would you handle a situation where a patient is demanding a prescription refill early?
First, I'd try to understand the patient's reason for needing the refill early. Is there a valid reason, such as lost medication or a change in their dosage prescribed by their doctor (requiring documentation). I would check the patient's prescription history and consult with the pharmacist to ensure the refill is safe and appropriate.
If there is no valid reason to refill, I would calmly and respectfully explain to the patient why I cannot fulfill their request at this time. I would explain the pharmacy's policy and legal guidelines regarding early refills. If the patient is still insistent, I would involve the pharmacist or my supervisor to help address the situation and find a solution.
23. What experience do you have with inventory management in a pharmacy setting?
In my previous role at [Pharmacy Name], I was actively involved in managing the pharmacy's inventory. This included tasks such as ordering medications and supplies based on demand forecasts and established par levels, receiving and verifying shipments against purchase orders, and accurately stocking shelves while adhering to FIFO (First-In, First-Out) principles to minimize waste and ensure product expiration dates were carefully monitored. I also regularly conducted cycle counts to reconcile physical inventory with system records, identifying and resolving any discrepancies.
Furthermore, I gained experience using [Pharmacy Inventory System Name] to track inventory levels, generate reports on stock usage, and identify potential shortages or overstock situations. I also assisted in managing the disposal of expired or recalled medications according to pharmacy protocols and regulatory guidelines.
24. Describe your experience with handling insurance claims and processing payments.
I have experience handling insurance claims from submission to resolution, including verifying policy coverage, investigating claim details, and assessing damages. My responsibilities included communicating with claimants, insurance adjusters, and other relevant parties to gather necessary information and documentation. I've also processed payments for approved claims, ensuring accurate and timely disbursement of funds, and adhering to established internal controls.
Specifically, I used systems for claim management, verifying policy details, updating statuses, and generating reports. I am familiar with standard insurance terminology, claim adjustment processes, and regulatory requirements related to claims processing.
25. How familiar are you with different dosage forms of medications (e.g., tablets, capsules, liquids)?
I have a good understanding of various medication dosage forms. I'm familiar with solid oral dosage forms like tablets (including immediate-release, extended-release, and enteric-coated), capsules (hard and soft gelatin), and powders. I also have knowledge of liquid dosage forms such as solutions, suspensions, and emulsions, as well as semi-solid forms like creams, ointments, and gels. Furthermore, I understand parenteral dosage forms (injections) and inhaled dosage forms (aerosols, inhalers).
My understanding includes the general formulation considerations, common excipients used, and the typical routes of administration for each dosage form. While I don't have hands-on experience in pharmaceutical compounding or manufacturing, I can analyze and process information related to these dosage forms effectively, which is helpful when processing data from clinical trials or analyzing prescription data.
26. What steps would you take to prevent medication errors in the pharmacy?
To prevent medication errors, I would focus on several key areas. First, meticulous verification is essential. This includes verifying the prescription's accuracy against the patient's profile, checking for allergies and drug interactions, and ensuring the correct drug, dosage, and route of administration are dispensed. Using technology like barcode scanning can aid in this process.
Second, clear communication is paramount. This involves actively listening to the patient, addressing any concerns they may have, and providing comprehensive counseling on the medication's purpose, dosage, potential side effects, and storage requirements. I would also advocate for a culture of open reporting, where staff feel comfortable reporting errors or near misses without fear of reprisal, enabling learning and system improvement.
27. How do you prioritize tasks when you have multiple responsibilities to manage?
When facing multiple responsibilities, I prioritize tasks using a combination of urgency and importance. I typically start by listing all my tasks and then assessing each based on these criteria. I use techniques like the Eisenhower Matrix (urgent/important) to categorize them. Urgent and important tasks get addressed first. Important but not urgent tasks are scheduled. Urgent but not important tasks are delegated if possible. Tasks that are neither urgent nor important are deferred or eliminated.
I also consider the impact and dependencies of each task. If a task is blocking others or has a significant impact on overall goals, it's given higher priority. I also communicate proactively with stakeholders to ensure alignment on priorities and to manage expectations.
28. What strategies do you use to manage stress in a fast-paced work environment?
In a fast-paced environment, I proactively manage stress using a few key strategies. First, I prioritize tasks ruthlessly, focusing on the most important items and delegating or deferring others when possible. I use techniques like the Eisenhower Matrix (urgent/important) to guide my decisions. Second, I incorporate short breaks throughout the day to detach and recharge; even a few minutes of mindfulness or a quick walk can make a big difference. I also ensure I maintain healthy habits outside of work, including regular exercise, sufficient sleep, and a balanced diet, as these significantly impact my resilience to stress. Finally, I communicate openly with my team and manager about workload and potential bottlenecks, seeking support and collaborating on solutions to prevent feeling overwhelmed.
29. Can you give an example of a time when you had to solve a problem creatively at work?
During a project, we encountered a performance bottleneck with a data processing script. The existing solution involved iterating through large datasets, which was time-consuming. To solve this creatively, I suggested leveraging Python's multiprocessing library to parallelize the processing. Instead of iterating through the data sequentially, we split the data into chunks and processed each chunk concurrently using multiple CPU cores.
This significantly reduced the processing time and improved overall performance. The initial attempts had locking issues when writing to the shared resources. After some debugging, I used Queue for message passing from the processes to the main thread. This facilitated thread-safe operation.
Intermediate Pharmacy Technician interview questions
1. Describe a time you identified a potential drug interaction. What steps did you take?
During a medication reconciliation, I noticed a patient was prescribed warfarin and also started on azithromycin by a different physician. Recognizing that azithromycin can increase the risk of bleeding in patients taking warfarin, I immediately flagged this potential interaction.
I first verified the interaction in a drug interaction database (Lexicomp). Then, I contacted the prescribing physician to discuss the interaction and alternative antibiotic options. I also informed the patient about the potential increased risk of bleeding and advised them to monitor for any signs of bleeding, such as unusual bruising or nosebleeds. The physician decided to switch the antibiotic to a safer alternative, and I documented the intervention in the patient's medical record.
2. How do you handle a situation where a patient is upset about a long wait time for their prescription?
I would first acknowledge the patient's frustration and apologize for the inconvenience caused by the long wait time. I would then try to understand the reason for the delay, explaining the situation to the patient clearly and honestly (e.g., "We're currently experiencing a high volume of prescriptions" or "There was an issue verifying your insurance").
Next, I would focus on finding a solution. This might involve checking the prescription status, expediting the process if possible, or offering alternatives like transferring the prescription to another pharmacy if appropriate and with their consent. I would actively listen to their concerns and ensure they feel heard and valued, demonstrating empathy and a willingness to help resolve the issue. I would also set realistic expectations about when the prescription will be ready.
3. Explain your experience with different pharmacy software systems. What are the pros and cons of each?
I have experience with several pharmacy software systems, including RxCelerate and PharmaPro. RxCelerate excels in inventory management and automated reordering, significantly reducing stockouts. However, its reporting features are somewhat limited, and the user interface can feel cluttered. PharmaPro offers robust reporting and analytics, providing valuable insights into prescription trends and patient adherence. The downside is that its inventory management module is less intuitive and requires more manual intervention.
Specifically with RxCelerate, the automatic dispensing feature increases efficiency, but the initial setup can be time-consuming and requires specialized training. PharmaPro's adherence monitoring tools are excellent for improving patient outcomes, but the system can be resource-intensive, requiring frequent updates and maintenance. My preference depends on the specific needs of the pharmacy; for high-volume dispensing and inventory control, RxCelerate is suitable. For detailed reporting and patient management, PharmaPro is better.
4. Tell me about a time you had to compound a medication. What were the challenges, and how did you overcome them?
During my pharmacy internship, I had to compound a topical cream for a patient with a specific allergy to a common preservative. The challenge was ensuring a sterile environment and precise measurements since the formulation was not commercially available. I meticulously cleaned and sanitized the compounding area, donned sterile gloves and a mask, and double-checked all calculations to minimize errors. Another challenge was ensuring the stability and homogeneity of the cream. To overcome this, I consulted the United States Pharmacopeia (USP) guidelines and used a high-quality mortar and pestle to ensure proper mixing and particle size reduction.
To further ensure the medication was accurately prepared, I asked a senior pharmacist to independently verify my calculations and the final product before dispensing it to the patient. We also provided the patient with clear instructions on storage and application, emphasizing the importance of keeping the cream away from heat and direct sunlight to maintain its stability. I learned the importance of attention to detail and adherence to strict protocols in compounding to ensure patient safety and medication efficacy.
5. How do you ensure accuracy when filling prescriptions with multiple medications and dosages?
When filling prescriptions with multiple medications and dosages, accuracy is paramount. I prioritize a systematic approach involving verification at each step. First, I carefully review the prescription details – patient name, medication names, dosages, frequency, and route of administration – against the patient's profile in the pharmacy system. This includes checking for allergies, drug interactions, and contraindications.
Next, I meticulously select the correct medications, verifying the NDC (National Drug Code) and expiration dates. I double-count medications, compare the dispensed amount with the prescribed quantity, and ensure the label accurately reflects all prescription details before dispensing. If anything is unclear, I immediately contact the prescriber for clarification. Furthermore, I counsel patients on proper medication usage, potential side effects, and storage instructions to promote adherence and prevent errors at home.
6. What is your understanding of HIPAA, and how do you maintain patient confidentiality in the pharmacy setting?
HIPAA, the Health Insurance Portability and Accountability Act, is a US law designed to protect patients' sensitive health information from being disclosed without their consent or knowledge. In a pharmacy setting, I understand this to mean being vigilant about safeguarding Protected Health Information (PHI). This includes things like patient names, addresses, medical conditions, medications, and payment information.
To maintain patient confidentiality, I would always verify a patient's identity before dispensing medication or discussing their health information. I would ensure all conversations are conducted discreetly and out of earshot of other patients. I'd properly dispose of any documents containing PHI, and adhere to all pharmacy policies and procedures regarding data security and HIPAA compliance. I would also be aware of potential HIPAA breaches and report them immediately to the appropriate personnel. Training and staying up-to-date on HIPAA regulations is also crucial.
7. Describe your experience with inventory management in a pharmacy. How do you minimize waste and stockouts?
In my pharmacy experience, I've managed inventory using both manual systems and electronic inventory management software. My responsibilities included ordering medications and supplies, receiving and verifying shipments, and stocking shelves while adhering to FIFO (First-In, First-Out) principles to minimize expiration-related waste. I also regularly conducted cycle counts to reconcile physical inventory with system records, identifying and resolving discrepancies promptly.
To minimize waste and prevent stockouts, I closely monitored medication usage patterns and adjusted ordering quantities accordingly. I also collaborated with pharmacists to identify slow-moving items and implement strategies to reduce their stock levels, such as offering alternative formulations or returning them to the supplier. Additionally, I tracked expiration dates meticulously and proactively addressed medications nearing expiration by dispensing them first or exploring options for donation where possible.
8. How do you prioritize tasks when you have multiple prescriptions to fill and patients waiting?
When faced with multiple prescriptions and waiting patients, I prioritize based on urgency and patient needs. First, I identify any STAT or immediate-release medications that require immediate attention. These take top priority. Next, I assess prescriptions that are time-sensitive, such as antibiotics or medications needed before discharge.
After addressing urgent needs, I prioritize remaining prescriptions based on a combination of factors, including patient wait time, complexity of the prescription, and any known patient-specific requirements (e.g., elderly patients, patients with mobility issues). I communicate with patients to manage expectations and keep them informed about the estimated wait times, and I also delegate tasks to pharmacy technicians or other staff members as needed to optimize efficiency.
9. What are some common pharmacy abbreviations, and how do you ensure you understand them correctly?
Common pharmacy abbreviations include 'bid' (twice a day), 'tid' (three times a day), 'qid' (four times a day), 'po' (by mouth), 'prn' (as needed), 'stat' (immediately), 'hs' (at bedtime), and 'Rx' (prescription). There are many more, and some can be error-prone if misinterpreted (like 'QD' for 'once daily' being mistaken for 'QID').
To ensure correct understanding, I always double-check the abbreviation against the full medication order or prescription. If there's any ambiguity, I immediately clarify with the prescribing physician or pharmacist. I also use readily available pharmacy reference materials and online databases to confirm the meaning of less common abbreviations, especially when dealing with unfamiliar medications or instructions. Consistency and verification are key to patient safety.
10. Explain the process of verifying a prescription with a doctor's office.
Verifying a prescription with a doctor's office typically involves several steps to ensure accuracy and patient safety. First, the pharmacy receives a prescription, either electronically, verbally, or as a hard copy. The pharmacist then reviews the prescription for completeness and any potential red flags, such as unusual dosages or drug interactions.
Next, the pharmacy staff contacts the doctor's office, usually by phone or electronic verification system, to confirm the prescription's details. They verify the patient's information, medication name, dosage, frequency, route of administration, and duration of therapy against the doctor's records. Any discrepancies are resolved with the doctor or their staff before dispensing the medication. Some jurisdictions may have specific regulations regarding the types of prescriptions that require verification or the methods of communication allowed.
11. How do you stay updated on new medications and changes in pharmacy regulations?
I stay updated on new medications and changes in pharmacy regulations through a combination of resources. This includes regularly reading publications from organizations like the FDA, DEA, and my state's Board of Pharmacy. I also subscribe to pharmacy journals and newsletters, and attend continuing education (CE) courses and conferences to learn about the latest developments and regulatory updates.
Additionally, I utilize online resources such as the National Association of Boards of Pharmacy (NABP) website and reputable drug information databases to research specific medications and regulations as needed. Staying connected with professional pharmacy organizations and colleagues also provides valuable insights and allows for discussion of current issues.
12. Describe a time you had to resolve a discrepancy between the prescription and the medication in stock.
In my previous role as a pharmacy technician, I encountered a situation where a patient's prescription was for amlodipine 5mg tablets, but we only had 2.5mg tablets in stock. I immediately brought this to the pharmacist's attention.
The pharmacist confirmed the discrepancy, and we contacted the prescribing doctor's office. It was determined that the patient could take two 2.5mg tablets to equal the prescribed 5mg dose. After receiving the doctor's explicit approval, I updated the prescription notes, carefully documented the change, and explained the situation and dosage instructions to the patient to ensure they understood how to take their medication correctly. This prevented any delay in the patient receiving their needed medication.
13. What is your experience with handling controlled substances, and what precautions do you take?
My experience with handling controlled substances involves strict adherence to established protocols and regulations. I understand the importance of accurate record-keeping, proper storage, and secure disposal methods. I have experience with inventory management systems designed to track controlled substances and prevent diversion.
My precautions include verifying prescriptions, confirming patient identity, and double-checking dosages. I always ensure that controlled substances are stored in locked cabinets or safes with limited access. I promptly report any discrepancies or suspected diversion to the appropriate authorities and follow established procedures for waste disposal to prevent misuse.
14. How do you handle a situation where a patient has questions about their medication that you are not qualified to answer?
If a patient asks a medication-related question I'm not qualified to answer, my priority is ensuring they receive accurate information. I would politely explain that I am not able to provide medical advice or specific details about medications.
I would then direct them to the appropriate resource, such as the prescribing physician, the pharmacist, or another qualified healthcare professional. I might say something like, "That's a great question, and it's important you get the right answer. I'm not able to give medical advice, so I recommend speaking with your doctor or the pharmacist who dispensed the medication. They can give you the most accurate and personalized information." I would also offer to help them contact the appropriate person if needed.
15. Tell me about a time you went above and beyond to help a patient.
During my time volunteering at a free clinic, I encountered a patient, Maria, who was recently diagnosed with diabetes but had limited resources and understanding of how to manage her condition. Beyond explaining her medication and diet, I took the initiative to connect her with a local food bank that provided diabetic-friendly options. I also spent extra time creating a simplified meal plan and demonstrating how to use a glucometer in Spanish, her primary language.
Furthermore, realizing she lacked transportation to follow-up appointments, I coordinated with a volunteer driving service to ensure she could attend. Weeks later, she shared that my support significantly improved her ability to manage her diabetes and reduced her anxiety about her health. This experience highlighted the importance of addressing the social determinants of health and reinforced my commitment to providing patient-centered care.
16. What strategies do you use to minimize errors in prescription filling?
To minimize errors in prescription filling, I use several strategies. First, I always double-check the prescription details against the patient's information, including allergies and current medications. I also verify the drug name, dosage, strength, and route of administration. Second, I employ techniques like reading the prescription aloud and comparing the medication label against the original prescription before dispensing. I also leverage pharmacy software and automated dispensing systems, which help flag potential drug interactions or incorrect dosages.
Furthermore, I maintain a clean and organized workspace to avoid distractions and mix-ups. I also proactively consult with the pharmacist when I have any questions or uncertainties about a prescription, prioritizing patient safety above all else.
17. Explain your understanding of different insurance plans and how they affect prescription processing.
Insurance plans, such as HMO, PPO, POS, and HDHP, impact prescription processing in various ways. HMOs typically require members to use in-network pharmacies and obtain referrals for specialists, potentially limiting choices and requiring prior authorizations for certain medications. PPOs offer more flexibility with out-of-network options but often have higher copays or deductibles. POS plans are a hybrid of HMO and PPO, requiring a primary care physician (PCP) but allowing out-of-network access, albeit with higher costs.
HDHPs, paired with Health Savings Accounts (HSAs), generally have lower premiums but higher deductibles, meaning members pay more out-of-pocket for prescriptions until the deductible is met. Formulary coverage, which drugs are covered and at what tier, also varies across plans and influences the price a patient pays. Furthermore, plans can impose quantity limits, step therapy requirements (trying a lower-cost drug first), and prior authorization requirements, all affecting the pharmacy's ability to process a prescription smoothly and the patient's access to medication.
18. How do you contribute to a positive team environment in the pharmacy?
I contribute to a positive team environment by being proactive, supportive, and respectful of my colleagues. I always offer assistance when I see someone struggling, whether it's helping to fill prescriptions, answering phones, or managing inventory. I believe open communication is crucial, so I actively listen to my teammates' concerns and ideas and share my own constructively.
Furthermore, I strive to maintain a positive attitude even during stressful situations. I acknowledge and appreciate the contributions of others and celebrate team successes. I am also committed to continuous learning and improvement and share my knowledge with others to foster a collaborative learning environment.
19. Describe your experience with aseptic technique. What are important steps?
My experience with aseptic technique primarily stems from laboratory work involving cell culture and microbiology. I understand the importance of preventing contamination in these environments. Key steps include: sterilizing equipment and media (usually via autoclaving), disinfecting work surfaces with appropriate solutions like 70% ethanol or bleach, using sterile supplies (pipettes, culture flasks, etc.), and employing proper hand hygiene techniques, including thorough hand washing and the use of sterile gloves. Working in a laminar flow hood is also crucial for maintaining a sterile work environment when handling sensitive materials.
Other important aspects are minimizing exposure time of sterile materials to the open air, employing "no touch" techniques where possible, and wearing appropriate personal protective equipment (PPE) like lab coats and masks. Furthermore, regular monitoring of aseptic technique through quality control measures (e.g., checking media for contamination) is essential to identify and address any potential breaches in protocol.
20. What steps would you take if you notice a coworker making a mistake that could harm a patient?
If I noticed a coworker making a mistake that could harm a patient, my immediate priority would be patient safety. First, I would directly and privately address the coworker about the mistake, explaining the potential harm it could cause. If the coworker acknowledges the mistake and takes immediate corrective action, I would monitor the situation to ensure the patient's safety.
However, if the coworker dismisses my concerns, refuses to correct the mistake, or if the situation presents an immediate and serious risk to the patient, I would escalate the issue to the appropriate authority, such as a supervisor or charge nurse. I would clearly and concisely explain the situation, the potential harm, and the steps I have already taken. My goal is to ensure that the mistake is corrected and the patient is protected, even if it means going over the coworker's head.
21. How do you handle a prescription that seems unusually high in dosage or quantity? What would you do?
If I receive a prescription that appears unusually high in dosage or quantity, my first step is to verify the prescription with the prescribing physician. I would contact the doctor's office directly, not relying solely on phone numbers on the prescription itself to prevent potential fraud. I would clearly and respectfully express my concerns about the dosage or quantity, asking the doctor to confirm the intended amount and frequency.
If the doctor confirms the prescription is accurate, I would still counsel the patient thoroughly about the medication, its potential side effects, and the importance of adhering to the prescribed dosage. I would also document the confirmation from the physician and the counseling session with the patient. If I'm unable to reach the prescriber, or if I have continued concerns after speaking with them, I would hold the prescription and discuss the situation with a senior pharmacist or my supervisor before dispensing.
Advanced Pharmacy Technician interview questions
1. Describe a time you identified a potential medication error. What steps did you take to resolve it?
During a routine chart review, I noticed a patient was prescribed warfarin and aspirin concurrently without a clear indication or documented justification. Knowing the increased risk of bleeding with this combination, I immediately consulted with the attending physician.
I explained my concern regarding the potential for increased bleeding risk. After reviewing the patient's history and current condition, the physician agreed with my assessment. The aspirin order was subsequently discontinued, and the patient was closely monitored for any signs of adverse effects. The incident was documented, and discussed during a team meeting to highlight the importance of vigilance regarding drug interactions.
2. How do you handle a situation where a pharmacist is unavailable and a patient needs urgent medication advice?
In the absence of a pharmacist, I would first assess the urgency of the patient's need. If it's a life-threatening situation, I would immediately call emergency services. If the situation is urgent but not life-threatening (e.g., severe allergic reaction, acute pain management), I would follow established protocols, which might involve contacting an on-call pharmacist or using pre-approved standing orders in consultation with a senior healthcare professional (e.g., a physician or nurse practitioner).
If the request is less urgent (e.g., a question about side effects or dosage of a non-critical medication), I would explain to the patient that the pharmacist is unavailable and that I can't provide medication advice. I would document the request and ensure the pharmacist addresses it as soon as they are available. I would also explore alternative options, such as directing the patient to reliable online resources or suggesting they contact their physician for immediate assistance.
3. Explain your experience with inventory management systems and strategies for minimizing waste.
I have experience working with inventory management systems (IMS) like NetSuite and smaller, custom-built systems. My experience includes tracking inventory levels, managing orders, and generating reports to analyze stock turnover and identify slow-moving items. I've used these systems to optimize warehouse layouts, implement cycle counting procedures, and improve overall inventory accuracy.
Regarding waste minimization, I've implemented strategies such as FIFO (First-In, First-Out) to reduce spoilage and obsolescence, especially important for perishable goods. I've also analyzed demand forecasts to optimize order quantities, preventing overstocking and minimizing storage costs. Furthermore, I worked on improving just-in-time inventory practices in order to reduce carrying costs.
4. Describe a complex compounding procedure you've performed. What were the key considerations?
During my time in a compounding pharmacy, I prepared hormone replacement therapy (HRT) capsules. This involved multiple active pharmaceutical ingredients (APIs) with varying potencies, particle sizes, and flow properties. Key considerations included ensuring accurate weighing of each API using calibrated balances, accounting for the potency of each API to achieve the correct final dosage per capsule, and selecting appropriate excipients like lactose monohydrate as a diluent and magnesium stearate as a lubricant to ensure uniform mixing and flowability of the powder blend. A geometrically increasing dilution method was employed to ensure proper mixing of the low potency APIs with the high potency ones.
Critical steps included meticulous documentation of each step in the compounding process as well as in-process testing to verify the blend uniformity using techniques like weight variation analysis and visual inspection. Proper cleaning and maintenance of the equipment (e.g., capsule filling machine, mortar and pestle, balances) were also vital to prevent cross-contamination. Finally, stability testing was implemented to determine the appropriate beyond-use date for the compounded capsules based on environmental conditions.
5. How would you approach training a new pharmacy technician on sterile compounding techniques?
I would approach training a new pharmacy technician on sterile compounding using a structured, multi-stage process. First, I'd begin with comprehensive didactic training, covering aseptic technique principles, relevant regulations (USP 797), calculations, and proper use of personal protective equipment (PPE). This would involve written materials, videos, and Q&A sessions.
Next, I'd move into hands-on training within a controlled environment, starting with simpler tasks like hand hygiene and garbing procedures. As the technician progresses, they would work their way up to compounding more complex preparations, always under direct supervision. Each step would involve demonstration, observation, and constructive feedback. Competency would be assessed through written exams, media fills, and direct observation of compounding activities until they meet the expected level of proficiency.
6. Explain your understanding of USP <797> and USP <800> standards and how you ensure compliance.
USP <797> focuses on sterile compounding, aiming to prevent harm to patients from contaminated compounded sterile preparations (CSPs). It outlines requirements for personnel training, facility design, environmental monitoring, storage, and documentation to ensure the quality and sterility of compounded medications. USP <800> specifically addresses the safe handling of hazardous drugs (HDs) to protect healthcare workers, patients, and the environment from exposure. It covers aspects like facility requirements, personnel training, personal protective equipment (PPE), spill management, and proper disposal of HDs.
To ensure compliance, I follow strict adherence to standard operating procedures (SOPs) derived from these guidelines. This includes undergoing regular training and competency assessments on aseptic techniques and HD handling. I meticulously document all compounding activities, environmental monitoring results, and personnel training records. Regular audits are conducted to identify any gaps in compliance and implement corrective actions. For HDs, I always use appropriate PPE, work within designated areas with proper ventilation, and follow established procedures for spill management and waste disposal. Continuous monitoring of compounding areas and HD storage is also crucial to maintain a safe and compliant environment.
7. How do you stay current with new medications, changes in pharmacy laws, and best practices in the field?
I stay current through a combination of professional resources and continuing education. I regularly read pharmacy journals like the Journal of the American Pharmacists Association and Pharmacy Times. I also subscribe to newsletters and email alerts from organizations like the FDA, DEA, and my state board of pharmacy to stay informed about regulatory changes and drug recalls.
Furthermore, I participate in continuing education (CE) programs, both online and at conferences, to learn about new medications, therapeutic updates, and evolving best practices. I also find value in discussions with colleagues and participation in professional pharmacy organizations to share knowledge and experiences.
8. Describe your experience with prior authorization processes. How do you navigate challenges in obtaining approvals?
In my previous roles, I've frequently interacted with prior authorization processes, primarily when working with [mention specific systems or insurance types]. My experience includes submitting authorization requests, appealing denials, and communicating with insurance companies and healthcare providers to gather necessary documentation. I'm familiar with using online portals and fax-based systems for submission.
When facing challenges in obtaining approvals, I prioritize clear and proactive communication. This involves thoroughly understanding the specific requirements of each payer, ensuring that the documentation is complete and accurate, and promptly addressing any questions or requests for additional information. When a denial occurs, I carefully review the reason for denial, consult with the provider, and prepare a well-supported appeal, citing relevant medical necessity criteria and clinical guidelines. I also proactively track the status of each request to ensure timely processing.
9. How do you handle a situation where a patient is visibly upset or angry about a prescription issue?
If a patient is upset, I would first remain calm and empathetic. I'd actively listen to understand their concerns without interruption, acknowledging their feelings with phrases like, "I understand your frustration." Next, I would investigate the issue thoroughly, checking the prescription details, insurance information, and inventory. I'd then explain the situation clearly and honestly, offering potential solutions. For example, if there's a coverage issue, I might suggest a discount card, a different formulation, or contacting their insurance company directly. If a mistake was made on our end, I would sincerely apologize and take immediate steps to correct it. Throughout the interaction, I would maintain a professional and respectful demeanor, focusing on resolving their problem efficiently and to the best of my ability.
If I cannot resolve the issue immediately, I would assure the patient that I will escalate the problem to a supervisor or appropriate resource and provide a timeline for follow-up. I would always prioritize patient satisfaction and safety, seeking assistance when needed to ensure a positive outcome.
10. Explain your knowledge of different types of insurance plans and their impact on prescription processing.
My understanding of insurance plans includes HMOs, PPOs, POS plans, and government-sponsored programs like Medicare and Medicaid. Each plan type impacts prescription processing differently. For instance, HMOs often require members to use in-network pharmacies and may need prior authorizations for certain medications, affecting claim adjudication. PPOs offer more flexibility in choosing pharmacies but might have higher copays. Medicare Part D involves formularies that dictate covered drugs and tiered pricing, influencing which medications are dispensed and at what cost. Medicaid programs vary by state, leading to diverse coverage rules and reimbursement rates.
Specifically relating to prescription processing, the plan dictates the formulary (a list of covered drugs), copays, deductibles, and prior authorization requirements. The pharmacy benefit manager (PBM) processes the claim based on the insurance plan's rules. Steps include verifying patient eligibility, checking the drug's formulary status, applying copays/deductibles, and adjudicating the claim. Rejected claims may occur due to non-covered drugs, exceeding quantity limits, or lacking prior authorization. Understanding these differences is crucial for efficient and accurate prescription fulfillment and billing.
11. Describe your experience with automated dispensing systems and their advantages and disadvantages.
I have experience working with automated dispensing systems (ADS) in a pharmacy setting. My role involved tasks such as loading medications into the system, troubleshooting minor technical issues, and managing inventory within the ADS. I also trained pharmacy staff on the proper use of the system and developed workflows to optimize its efficiency.
The advantages of ADS include increased dispensing accuracy, reduced medication errors, faster prescription processing times, and improved inventory management. Disadvantages can include high initial costs, potential for mechanical failures, the need for ongoing maintenance and calibration, and a dependency on the system that can disrupt workflows during downtime. I have also observed that some systems can be inflexible regarding packaging sizes or medication formulations, requiring manual dispensing in certain cases.
12. How would you handle a recall situation, ensuring all affected medications are identified and removed from circulation?
In a recall situation, I would immediately follow established protocols, prioritizing patient safety. The first step involves identifying all affected medications using lot numbers, expiration dates, and any other identifying information provided in the recall notice. This requires a thorough search of inventory databases, dispensing records, and potentially physical stock checks within the pharmacy or healthcare facility.
Next, I would quarantine all identified medications to prevent further dispensing. This includes physically removing them from shelves and clearly marking them as recalled. We would then notify patients who received the recalled medication, following communication guidelines provided by the regulatory bodies or the manufacturer. Finally, we would document all actions taken, including the number of units recalled, the dates of removal, and any patient communication records, adhering to recall procedures and guidelines.
13. Explain your understanding of medication synchronization programs and their benefits for patients.
Medication synchronization programs, often called "med sync," are services offered by pharmacies to coordinate a patient's multiple prescriptions so they can be refilled on the same day each month. This simplifies medication management for patients, reducing the number of trips to the pharmacy and improving adherence to prescribed regimens.
The benefits for patients are numerous. These include increased convenience, improved adherence leading to better health outcomes, enhanced communication with pharmacists about their medications, and reduced risk of running out of essential medications. By consolidating refills, patients are more likely to take their medications as prescribed, leading to better control of chronic conditions and fewer hospitalizations. It's a patient-centric approach to pharmacy care.
14. How do you prioritize tasks in a fast-paced pharmacy environment with multiple competing demands?
In a fast-paced pharmacy, I prioritize tasks based on urgency and importance, focusing on patient safety first. I quickly assess each request, identifying prescriptions that need immediate attention (e.g., STAT orders, antibiotics), potential drug interactions, or patients requiring counseling. Tasks are then addressed in the following order: safety concerns, urgent prescriptions, routine prescriptions, inventory management, and administrative tasks.
Communication is key, so I keep the team informed of my priorities and any potential delays. I also leverage available resources, such as pharmacy technicians, to delegate tasks effectively. Regularly reassessing the workload allows for adjustments to be made throughout the day as new requests come in or priorities shift. I always aim to prevent errors and maintain a smooth workflow.
15. Describe your experience with managing controlled substances and ensuring proper record-keeping.
During my time at [Previous Company/Role], I was responsible for managing controlled substances, specifically [mention specific substances if applicable, e.g., schedule II opioids]. This involved adhering to strict DEA and state regulations for procurement, storage, dispensing, and disposal. I maintained meticulous records, including inventory logs, dispensing records, and disposal documentation, ensuring accurate tracking and accountability.
I implemented [mention specific systems or processes, e.g., a double-signature system for dispensing, regular inventory audits] to prevent diversion and ensure compliance. I also conducted regular training for staff on proper handling procedures and record-keeping requirements. Any discrepancies were immediately investigated and reported according to established protocols.
16. How would you approach implementing a new pharmacy software system or process change?
First, I'd focus on gathering comprehensive requirements by collaborating with all stakeholders (pharmacists, technicians, IT staff, management) to understand their needs and pain points. This includes analyzing current workflows, identifying areas for improvement, and defining specific goals for the new system or process change. Crucially, I'd prioritize patient safety and regulatory compliance (HIPAA, etc.).
Next, I would develop a detailed implementation plan that addresses data migration, system configuration, user training, testing, and go-live support. This plan would include clear timelines, assigned responsibilities, and risk mitigation strategies. Pilot programs with a small group of users are useful to identify and resolve any issues before a full rollout. Post-implementation, continuous monitoring and evaluation are essential to ensure the system is performing as expected and meeting the defined goals. User feedback should be gathered regularly for ongoing optimization and improvement.
17. Explain your understanding of HIPAA regulations and how you protect patient privacy in the pharmacy setting.
HIPAA, the Health Insurance Portability and Accountability Act, establishes national standards to protect individuals' medical records and other personal health information (PHI). My understanding includes the Privacy Rule, which governs the use and disclosure of PHI; the Security Rule, which mandates safeguards for electronic PHI; and the Breach Notification Rule, requiring reporting of breaches of unsecured PHI. In a pharmacy setting, I protect patient privacy by verifying patient identity before dispensing medications, counseling, or accessing records. I ensure prescriptions are handled discreetly, avoid discussing patient information in public areas, and securely store patient records both physically and electronically.
Furthermore, I am vigilant about adhering to pharmacy policies and procedures related to HIPAA. This includes only accessing patient information that is necessary for my job duties (minimum necessary standard), using secure communication methods for transmitting PHI (e.g., encrypted email), and promptly reporting any suspected breaches of privacy or security to the designated HIPAA compliance officer. Regular training and updates on HIPAA regulations are vital to staying informed and maintaining compliance.
18. How do you handle a situation where you disagree with a pharmacist's decision regarding a prescription?
If I disagree with a pharmacist's decision about a prescription, I would first calmly and respectfully discuss my concerns with them, providing the reasoning behind my perspective and backing it up with evidence-based information, such as clinical guidelines or relevant studies. My priority is patient safety, so I would try to understand the pharmacist's rationale and see if there's a misunderstanding or if new information can change the decision.
If, after a thorough discussion, I still believe the decision poses a risk to the patient, I would escalate the issue to a more senior pharmacist or a medical director, following the appropriate channels and documenting all steps taken. My goal is to ensure the best possible outcome for the patient while maintaining a professional and collaborative relationship with my colleagues. Ultimately, patient well-being always takes precedence.
19. Describe your experience with working with different healthcare providers and communicating patient information effectively.
Throughout my experience, I've collaborated with a diverse range of healthcare providers, including physicians, nurses, therapists, and specialists. My communication strategy prioritizes clarity, accuracy, and adherence to HIPAA guidelines. I ensure patient information is shared securely and efficiently using various methods.
Specifically, I've utilized electronic health record (EHR) systems to document and access patient data, actively participating in interdisciplinary team meetings to discuss patient progress and care plans. I am adept at conveying complex medical information in a manner easily understood by both clinical and non-clinical staff, improving the overall team communication.
20. How do you contribute to a positive and collaborative work environment in the pharmacy?
I contribute to a positive pharmacy environment by actively communicating and supporting my colleagues. This involves being approachable, offering assistance when needed, and proactively sharing relevant information, such as updates on drug shortages or changes in protocols. I also prioritize clear and respectful communication, especially when addressing concerns or resolving conflicts.
Furthermore, I believe in fostering a collaborative atmosphere through teamwork and shared responsibility. This includes participating in team meetings, openly discussing ideas and potential solutions, and being receptive to feedback from others. I am committed to maintaining a professional attitude and contributing to a culture of continuous improvement within the pharmacy setting.
21. Explain your understanding of medication adherence and strategies for improving patient compliance.
Medication adherence refers to the extent to which a patient's behavior aligns with the prescribed recommendations from a healthcare provider regarding medication intake. This includes factors such as dosage, timing, and frequency. Poor adherence can lead to suboptimal treatment outcomes, increased healthcare costs, and disease progression.
Strategies to improve patient compliance involve a multi-faceted approach. These include:
- Education: Providing clear and concise information about the medication, its purpose, potential side effects, and proper administration.
- Simplification: Reducing the complexity of the medication regimen, perhaps through combination pills or fewer doses.
- Reminders: Utilizing tools like pill organizers, alarms, or mobile apps to remind patients to take their medication.
- Communication: Fostering open communication between the patient and healthcare provider to address concerns and barriers to adherence.
- Support: Involving family members or caregivers to provide support and encouragement. Regular follow-ups and monitoring can also improve compliance.
22. How do you handle a situation where you suspect a patient is doctor shopping or misusing medications?
If I suspect a patient is doctor shopping or misusing medications, my first step is always to gather more information. I would carefully review the patient's medical history, paying attention to prescription records and past consultations. I would also have an open and honest conversation with the patient, expressing my concerns in a non-judgmental way and giving them an opportunity to explain their perspective.
If my suspicions remain after these steps, I would consult with senior colleagues, pharmacists, and potentially the medical board or relevant regulatory agencies, adhering to established protocols and legal requirements. Patient safety and well-being are paramount, but it's crucial to balance this with respecting patient privacy and avoiding unwarranted accusations. Documentation of concerns and actions taken is also essential.
23. Describe your experience with handling hazardous medications and ensuring safety for yourself and others.
During my time as a pharmacy technician and while volunteering at a local hospital, I gained experience handling hazardous medications, primarily chemotherapy drugs and certain antivirals. My training included comprehensive protocols for personal protective equipment (PPE) such as double gloving, wearing gowns, and using respirators when compounding. I followed strict procedures for preparation in designated areas with proper ventilation, and I meticulously labeled and stored medications according to safety guidelines.
I was also responsible for the safe disposal of hazardous waste, including unused medications and contaminated materials, using designated containers and following waste management protocols. I actively participated in regular safety training sessions and remained updated on any changes to handling procedures. I was trained on spill management and decontamination, including where to find the relevant supplies and documentation. I’ve also actively encouraged colleagues to adhere to safety protocols, promptly addressing any observed deviations to ensure a safe environment for everyone.
24. How would you approach a situation where a patient is unable to afford their medication?
If a patient is unable to afford their medication, I would first empathetically acknowledge their concern and assure them I want to help find a solution. I would then explore the following options:
- Check for generic alternatives: Determine if a more affordable generic version of the medication is available and suitable for the patient.
- Investigate patient assistance programs (PAPs): Research whether the pharmaceutical company that manufactures the medication offers a patient assistance program that could provide the medication at a reduced cost or for free.
- Explore other financial aid programs: Look into programs like Medicaid, Medicare Extra Help, or other local and national assistance programs that can help with medication costs.
- Discuss alternative treatment options: Consult with the prescribing physician to see if there are equally effective but less expensive alternative medications or treatment plans.
- Offer a discount card (if applicable): Inform the patient about any available discount cards or coupons that can lower the price of the medication.
Throughout this process, maintaining open communication with both the patient and the physician is crucial to ensure the best possible outcome within the patient's financial constraints.
25. Explain your knowledge of different dosage forms and routes of administration, and their implications for patient care.
Dosage forms are the physical forms of a medication, influencing how a drug is administered and absorbed. Common examples include tablets, capsules, liquids, creams, injections, and inhalers. The route of administration refers to how the drug enters the body (e.g., oral, intravenous, topical, intramuscular, subcutaneous). The choice of dosage form and route significantly impacts patient care by affecting the drug's bioavailability (the rate and extent to which a drug reaches systemic circulation), onset of action, duration of effect, and potential for side effects. For example, intravenous administration provides rapid and complete bioavailability, useful in emergencies, while oral administration is more convenient but subject to first-pass metabolism, reducing bioavailability.
Understanding these factors is crucial for healthcare professionals to select the most appropriate dosage form and route based on the patient's condition, age, ability to swallow, and other individual characteristics. Incorrect choices can lead to treatment failure, adverse reactions, or unnecessary patient discomfort. For instance, a patient with nausea and vomiting might not be able to take oral medication, requiring an alternative route like intravenous or rectal administration. Similarly, the extended-release formulation may improve patient compliance by reducing the frequency of dosing.
26. How do you ensure accuracy and efficiency when filling a high volume of prescriptions?
To ensure accuracy and efficiency when filling a high volume of prescriptions, I would prioritize a multi-faceted approach. First, implement robust verification steps at each stage: prescription entry, drug selection, compounding (if applicable), and final dispensing. This includes utilizing barcode scanning to verify medication and dosage, and double-checking calculations. Second, optimize workflow and leverage automation where possible. This can include automated dispensing systems (ADS) and efficient inventory management. Finally, provide thorough training to pharmacy staff on standard operating procedures and emphasize the importance of clear communication and teamwork to minimize errors and maximize throughput.
27. Describe a time you went above and beyond to help a patient. What was the situation and what did you do?
During a particularly busy shift, I noticed a patient, Mrs. Davis, who was visibly anxious and upset. She was scheduled for a complex procedure and was alone, with no family present. I spent extra time with her, explaining the procedure in detail, answering her questions patiently, and offering reassurance. I also learned that her anxiety stemmed from concerns about managing her pet at home post-surgery. I contacted the hospital's volunteer services and arranged for a volunteer to visit her home daily to care for her pet during her recovery.
Beyond just addressing her medical concerns, I wanted to ease her worries about her personal life so she could focus on recovery. Mrs. Davis was incredibly grateful, and her demeanor visibly improved. Knowing I made a positive difference in her overall well-being, not just her medical condition, was very rewarding.
Expert Pharmacy Technician interview questions
1. Describe a time you identified a potential medication error. What steps did you take to rectify it, and what was the outcome?
During my pharmacy rotation, I noticed a prescription for a patient with renal impairment for a standard dose of Vancomycin. Knowing that Vancomycin is nephrotoxic and requires dose adjustments based on renal function, I reviewed the patient's lab results and found their creatinine clearance was significantly lower than normal.
I immediately brought my concern to the supervising pharmacist. We collaborated to contact the prescribing physician and suggested a lower Vancomycin dose based on the patient's creatinine clearance. The physician agreed, and the prescription was adjusted. This prevented potential kidney damage in the patient. I also documented the intervention in the patient's chart.
2. How do you stay updated with the latest advancements in pharmaceutical technology and regulations?
I stay updated through a combination of industry-specific and general awareness strategies. This includes regularly reading reputable pharmaceutical journals like "Nature Reviews Drug Discovery" and publications from regulatory bodies such as the FDA and EMA.
I also actively participate in industry conferences, webinars, and online forums dedicated to pharmaceutical technology. Following key opinion leaders and relevant organizations on social media (LinkedIn, Twitter) provides real-time insights into emerging trends and regulatory changes. Finally, I subscribe to newsletters that curate relevant articles and updates from various sources.
3. Explain your experience with inventory management systems and strategies to minimize waste and prevent shortages.
In my previous role, I actively utilized inventory management systems like NetSuite and Fishbowl Inventory to track stock levels, manage purchase orders, and analyze sales trends. I implemented strategies such as ABC analysis to prioritize high-value items and optimize safety stock levels to prevent shortages. Regular cycle counts and physical inventory checks were crucial for maintaining data accuracy. I also collaborated with the sales and marketing teams to forecast demand and adjust inventory levels accordingly.
To minimize waste, I focused on reducing obsolete inventory through promotions and clearance sales. I also implemented a FIFO (First-In, First-Out) system to ensure that older items were used or sold first. This involved careful monitoring of expiration dates and proactive planning to avoid spoilage or obsolescence. Analyzing vendor lead times and implementing just-in-time (JIT) inventory practices, where feasible, also helped to reduce holding costs and waste.
4. What strategies do you employ to handle difficult or demanding patients while maintaining professionalism and accuracy?
When faced with difficult or demanding patients, I prioritize active listening and empathy. I try to understand their concerns and validate their feelings, even if I don't agree with their behavior. This involves maintaining a calm and respectful demeanor, speaking in a clear and reassuring tone, and avoiding defensiveness. I focus on finding solutions to their immediate concerns and setting realistic expectations while adhering to established protocols and ethical guidelines.
If a situation escalates, I may involve a supervisor or colleague for assistance. Documenting all interactions thoroughly is crucial for maintaining accuracy and providing a clear record of the events. Setting professional boundaries is also important to prevent burnout and ensure I can continue providing quality care to all patients.
5. Describe your experience with compounding medications, including any specialized training or certifications.
My experience with compounding medications includes preparing various non-sterile compounds such as creams, ointments, solutions, and suspensions, following established formulations and standard operating procedures. I have experience using equipment like electronic balances, mortar and pestle, and ointment mills. I also have experience performing calculations related to compounding, including alligations and conversions. While I don't have specific specialized certifications in compounding, I have completed several continuing education courses focused on pharmaceutical compounding best practices and USP guidelines, especially USP 795. I am also familiar with documentation requirements, including compounding records and master formulation records.
6. How do you ensure accuracy when processing a high volume of prescriptions under strict time constraints?
To ensure accuracy when processing a high volume of prescriptions under strict time constraints, I would prioritize a multi-faceted approach. First, standardize the workflow using checklists and templates to minimize errors and improve speed. Implement technology such as barcode scanners and automated dispensing systems to reduce manual data entry and verification steps. Regular training and competency assessments for pharmacy staff are also crucial.
Second, incorporate redundant verification steps. This includes pharmacist review of all prescriptions, double-checking dosages and patient information, and using software with built-in error detection. Prioritize critical prescriptions based on urgency and complexity to ensure timely and accurate processing. Effective communication and collaboration among the pharmacy team are also essential to prevent mistakes and maintain a safe working environment. Finally, perform regular audits of the prescription processing workflow to identify areas for improvement and implement corrective actions.
7. Can you share an example of when you had to troubleshoot a complex insurance claim issue? What was your approach?
In a prior role, I encountered a complex claim involving multiple vehicles and disputed liability after a major highway accident. The initial assessment was unclear due to conflicting police reports and witness statements. My approach began with gathering all available information, including the claim file, police reports, witness statements, and policy details of all involved parties. Then, I carefully analyzed the information, identifying inconsistencies and gaps in the evidence. I conducted follow-up interviews with the claimants and witnesses to clarify details and address discrepancies.
Following data collection, I consulted with our legal team to assess the legal implications of each party's potential liability. I also worked with a claims adjuster experienced in accident reconstruction to perform a detailed analysis of the accident scene. Through meticulous investigation and expert consultation, we were able to establish a clearer picture of the events and determine the appropriate allocation of liability. This resulted in a fair settlement for all involved parties, avoiding lengthy and costly litigation.
8. Explain your understanding of HIPAA regulations and how you maintain patient confidentiality in your daily tasks.
HIPAA, the Health Insurance Portability and Accountability Act, establishes national standards to protect individuals' medical records and other personal health information. My understanding includes the Privacy Rule, which governs the use and disclosure of protected health information (PHI); the Security Rule, which outlines administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic PHI; and the Breach Notification Rule, requiring notification to affected individuals and HHS in the event of a breach of unsecured PHI.
In my daily tasks, I maintain patient confidentiality by adhering to strict protocols. These include using encrypted communication channels for any transmission of PHI, accessing patient data only on a need-to-know basis, properly disposing of documents containing PHI, and ensuring physical security measures are in place to prevent unauthorized access to patient information. I'm also very careful when discussing patient information to avoid incidental disclosures. I'm committed to continuous learning about updates to HIPAA regulations to remain compliant.
9. Describe a time when you had to train a new pharmacy technician. What methods did you use to ensure their success?
When a new pharmacy technician joined our team, I took a structured approach to their training. First, I focused on the fundamental aspects: prescription intake procedures, understanding common medications, and using our pharmacy software. I would demonstrate a task, then have them perform it under my direct supervision, providing immediate feedback and correction. We utilized a checklist to ensure all key areas were covered, and I encouraged them to ask questions, fostering an open and comfortable learning environment.
To gauge their progress and reinforce learning, I incorporated quizzes and practical exercises. For example, I’d simulate prescription scenarios and have them process them from start to finish. I also paired them with more experienced technicians for shadowing and peer support. Regular check-ins allowed me to address any challenges they were facing and tailor my approach accordingly. Ultimately, my goal was to empower them with the knowledge and confidence needed to excel in their role, contributing to efficient and safe pharmacy operations.
10. How do you prioritize tasks in a fast-paced pharmacy environment, especially when faced with conflicting demands?
In a fast-paced pharmacy, prioritization is crucial. I would first assess the urgency and importance of each task. Patient safety is always the top priority, so prescriptions that are needed immediately or involve critical medications (like antibiotics or insulin) take precedence. Then, I'd triage based on a combination of factors: prescriptions that are 'promised' for a particular time, doctor's requests, legal requirements, and inventory needs to avoid outages.
When conflicting demands arise, clear communication is key. I would calmly and professionally communicate with both the patients/doctors/colleagues and explain the situation, outlining the reasons for the prioritization. If necessary, I will ask for help from senior colleagues or pharmacists to ensure every task is handled efficiently and safely and also make sure no task is left unattended.
11. What is your experience with automated dispensing systems, and how do you ensure their accuracy and efficiency?
I have experience working with automated dispensing systems in a [pharmacy/hospital - specify context]. My primary focus has been on ensuring accuracy and efficiency through several key strategies. This includes regular calibration and maintenance of the systems according to manufacturer guidelines, and implementing robust verification protocols, such as barcode scanning and weight checks, to minimize dispensing errors.
Beyond these steps, I have also focused on optimizing system workflows to reduce processing time. This includes properly stocking the machines and managing inventory levels to avoid delays, and proactively identifying and addressing any bottlenecks in the dispensing process. My experience extends to training staff on proper system usage and troubleshooting common issues to maximize efficiency and minimize downtime.
12. Explain how you would handle a situation where a patient is requesting a refill that is not yet due according to their insurance plan.
When a patient requests a refill that isn't yet covered by their insurance, I would first verify the refill date and insurance policy details to confirm the denial. I would then explain the situation clearly and empathetically to the patient, outlining why the refill is not yet covered according to their insurance plan. I'd explore alternative options such as: checking if an override is possible with the insurance company (often requires physician authorization), offering a short-term supply to bridge the gap until the refill is covered, or discussing cash-pay options for the prescription. Finally, I'd document the interaction and the chosen course of action in the patient's record.
If the patient remains dissatisfied, I would involve the pharmacist or pharmacy manager to explore additional solutions. It's important to maintain a balance between adhering to insurance regulations and providing the best possible patient care. Communication and transparency are key to managing these situations effectively.
13. Describe your experience with managing controlled substances, including inventory tracking and security protocols.
During my time at [Previous Company/Role], I was responsible for managing controlled substances, ensuring strict compliance with DEA regulations. This involved meticulous inventory tracking using [Specific Software/System Used, e.g., a pharmacy management system or a dedicated inventory database]. I performed regular stock checks, reconciled inventory against prescriptions and usage logs, and investigated any discrepancies immediately.
Security protocols were a top priority. Access to controlled substances was restricted to authorized personnel only, and storage areas were secured with [Specific Security Measures, e.g., locked cabinets, alarm systems, surveillance cameras]. I also oversaw the proper disposal of expired or unused substances according to established procedures and maintained detailed records of all transactions, audits and disposals for compliance purposes. I also participated in routine internal audits and external DEA inspections, ensuring that all processes were fully compliant with regulatory requirements.
14. How do you handle a situation where you suspect a prescription may be fraudulent or altered?
If I suspect a prescription is fraudulent or altered, my priority is patient safety and adhering to legal/ethical guidelines. I would first carefully examine the prescription for common signs of forgery, such as unusual handwriting, altered quantities, mismatched information (e.g., date and medication appropriateness), and suspicious photocopies. I would then attempt to verify the prescription with the prescribing physician's office directly, using a known phone number and documenting the conversation.
If unable to verify, or if my suspicions remain, I would withhold dispensing the medication and inform the pharmacist-in-charge or pharmacy manager immediately. A detailed incident report would be filed, and depending on the severity and local regulations, the appropriate authorities (e.g., local police, state board of pharmacy) might be notified. Under no circumstances would I dispense a medication if I have reasonable doubt about the prescription's authenticity.
15. What strategies do you use to minimize medication errors related to look-alike/sound-alike drugs?
To minimize medication errors related to look-alike/sound-alike (LASA) drugs, I employ several strategies. First, I always double-check the drug name, dosage, and route of administration against the original prescription. Paying close attention to the spelling and using tall man lettering (e.g., buPROPion vs. busPIRone) where available helps to visually differentiate similar drug names. I also utilize barcode scanning during dispensing to ensure the correct medication is selected.
Furthermore, I actively maintain awareness of common LASA drug pairs by consulting resources like ISMP (Institute for Safe Medication Practices) lists. When prescribing or dispensing, I include the indication for use on the prescription to provide additional clarification. I also encourage patients to ask questions about their medications and verify the drug name and dosage with them during counseling. Finally, I report any potential LASA errors or near misses to facilitate continuous improvement in medication safety practices.
16. Explain your understanding of different pharmacy software systems and your ability to adapt to new technologies.
I understand that pharmacy software systems are crucial for managing prescriptions, inventory, patient records, and billing. I'm familiar with common types like dispensing software (e.g., Rx30, PioneerRx), inventory management systems, and pharmacy information systems that integrate various functions. My experience includes hands-on work with [mention specific systems if applicable], where I performed tasks such as data entry, prescription processing, inventory tracking, and generating reports.
I'm confident in my ability to adapt to new technologies. I have a strong foundation in computer literacy, and I'm a quick learner. I approach new software by first understanding its core functionalities and then practicing with it. I also utilize available resources like user manuals, online tutorials, and vendor support to become proficient. In my previous roles, I successfully learned and implemented [mention a specific software or technology] within a short timeframe, which demonstrates my adaptability. I also keep abreast of changes and updates related to pharmacy software by attending webinars, reading industry publications, and participating in relevant online forums.
17. Describe a time you had to resolve a conflict with a coworker in the pharmacy setting. What was your approach?
In a busy pharmacy, I noticed a growing tension between two technicians regarding task assignments. One felt consistently burdened with filling prescriptions while the other primarily handled customer service. I initiated a private conversation with each of them to understand their perspectives. I discovered that the technician filling prescriptions felt undervalued and overwhelmed, while the customer service technician felt less confident in filling complex prescriptions.
To resolve this, I proposed a structured cross-training program. I created a schedule where each technician would spend dedicated time shadowing the other, learning their respective roles. We also had a team meeting to openly discuss workload distribution and individual skill sets. By creating a more balanced and supportive environment, the conflict dissipated, leading to improved teamwork and efficiency in the pharmacy.
18. How do you handle patient inquiries about over-the-counter medications and provide appropriate recommendations?
When a patient inquires about over-the-counter (OTC) medications, I first gather information about their symptoms, medical history, and any current medications they're taking, including allergies and existing conditions. This helps identify potential contraindications or interactions. I then use my knowledge of pharmacology and common OTC medications to suggest appropriate options, explaining the mechanism of action, dosage, potential side effects, and any necessary precautions. I emphasize the importance of reading and following the product label.
I always advise patients that I am not a medical professional, and to seek advice from a doctor or pharmacist. When appropriate, I also suggest non-pharmacological approaches, such as lifestyle modifications, and encourage them to seek professional medical advice if their symptoms worsen or persist. I also point out available resources like the National Institute of Health and patient education materials provided by the pharmaceutical manufacturers. It is also important to document these conversations.
19. What steps do you take to ensure proper disposal of hazardous waste and expired medications in the pharmacy?
To ensure proper disposal of hazardous waste and expired medications, I follow these steps: First, I segregate expired medications and hazardous waste from regular trash. Expired medications are placed in designated bins for return to a reverse distributor or for destruction via incineration, depending on pharmacy policy and DEA regulations. For hazardous waste, which includes items like chemotherapy drugs or certain creams, I carefully follow the guidelines outlined by the EPA and our pharmacy's hazardous waste management plan. This often involves using specific containers, labeling them correctly with details like contents and accumulation start date, and storing them in a secure location until a licensed waste disposal company can collect them.
Documentation is crucial. I maintain detailed records of all disposed medications and hazardous waste, including dates, quantities, and the method of disposal. These records are essential for compliance with regulatory requirements and for tracking waste management practices within the pharmacy. I also ensure that all staff members are properly trained on hazardous waste disposal procedures and understand the importance of following these protocols to protect the environment and public health.
20. Explain your experience with sterile compounding techniques and adherence to USP 797 standards.
During my experience, I've worked extensively with sterile compounding, ensuring strict adherence to USP 797 standards. This involved preparing both sterile and non-sterile medications, including IV admixtures, ophthalmic solutions, and other injectables, within ISO Class 5 environments, typically using laminar airflow workbenches (LAFWs) or compounding aseptic isolators (CAIs). Key aspects of my work included performing calculations and measurements accurately, using aseptic techniques to minimize contamination, and documenting all steps of the compounding process meticulously.
I’ve also been responsible for environmental monitoring, cleaning and disinfection of the compounding areas, and regular testing of personnel competency in aseptic techniques through media fills. My focus was always on maintaining a safe and sterile environment to protect patients from harm. Understanding the importance of proper garbing, hand hygiene, and airflow dynamics within the cleanroom were crucial aspects of my daily routine.
21. Describe a time when you went above and beyond to provide exceptional customer service to a patient.
During a particularly busy flu season, I noticed an elderly patient looking confused and overwhelmed after receiving her vaccination. She mentioned that she lived alone and was worried about managing her symptoms if she felt unwell. Although it wasn't strictly part of my role, I took the time to explain in detail how to manage potential side effects, provided her with written instructions, and even called a local volunteer organization that provides meal delivery and check-in services for seniors. I also personally followed up with her the next day to ensure she was feeling okay.
She was incredibly grateful for the extra care and attention. Her daughter later called to express her appreciation, saying it had given her immense peace of mind knowing her mother was being looked after. This experience reinforced my belief that even small acts of kindness can make a significant difference in a patient's well-being and overall experience.
22. How do you stay motivated and engaged in your work, even during challenging or stressful periods?
During challenging periods, I focus on breaking down large tasks into smaller, more manageable goals. This allows me to see progress and maintain a sense of accomplishment. I also prioritize self-care, ensuring I get enough rest, exercise, and time for activities I enjoy. This helps me recharge and approach challenges with a fresh perspective.
To stay engaged, I actively seek opportunities for learning and growth, whether it's through online courses, attending workshops, or collaborating with colleagues. I also find it helpful to connect with the broader purpose of my work and remind myself how my contributions are making a difference. When possible, I look for ways to introduce novelty or creativity into my tasks to prevent burnout. Regular reflection on my accomplishments and areas for improvement also motivates me to continuously refine my skills and approach to work.
23. What role do you see pharmacy technicians playing in the future of healthcare?
Pharmacy technicians will play an increasingly vital role in the future of healthcare, driven by factors like an aging population and a greater emphasis on preventative care. They'll likely take on more responsibility for tasks such as medication reconciliation, patient education, and adherence monitoring, freeing up pharmacists to focus on more complex clinical duties.
Increased automation and technological advancements will also change the landscape. Pharmacy technicians will need to be proficient in using new technologies, managing automated dispensing systems, and potentially even assisting with tasks like compounding personalized medications or administering vaccines under supervision. Their role will evolve towards a more patient-centered and technologically integrated one, becoming critical members of the healthcare team.
24. Explain your understanding of the different types of prescription drug insurance plans and their common requirements.
Prescription drug insurance plans, such as those offered under Medicare Part D or through private insurance, typically fall into a few main categories. Common types include: copay plans (where you pay a fixed amount per prescription), coinsurance plans (where you pay a percentage of the drug cost), and deductible plans (where you must meet a certain out-of-pocket expense before the insurance starts covering costs). Some plans may also feature a tiered formulary, meaning different drugs have different cost-sharing levels based on their classification (e.g., generic, preferred brand, non-preferred brand, specialty).
Common requirements across these plans often involve a formulary, which is a list of covered drugs; prior authorization, where the insurance company needs to approve certain medications before they are covered; step therapy, which requires trying a lower-cost drug before a more expensive one; and quantity limits, which restrict the amount of medication dispensed at one time. Understanding these elements is critical for navigating prescription drug coverage effectively.
25. Describe your experience with prior authorizations and the steps involved in obtaining them.
In my previous roles, I've frequently encountered prior authorizations, especially while working with pharmacy benefit managers (PBMs) and healthcare providers. My experience involves understanding payer-specific requirements, navigating online portals, and communicating with both healthcare professionals and insurance companies. The general process includes verifying patient eligibility and insurance coverage, reviewing the prescribed medication or service against the payer's formulary and guidelines, and gathering the necessary clinical documentation (e.g., medical records, lab results, physician notes) to support the request.
The specific steps usually entail:
- Submitting the prior authorization request through the payer's online portal or via fax.
- Following up on the status of the request.
- Addressing any queries or denials by providing additional information or appealing the decision.
- Documenting all communication and actions taken in the patient's record.
26. How would you address a situation where a patient is experiencing an adverse reaction to a medication?
If a patient is experiencing an adverse reaction to medication, my immediate priority is to ensure the patient's safety and well-being. I would first assess the severity of the reaction by monitoring vital signs and observing the patient's symptoms. I would then immediately notify the appropriate medical personnel, such as the attending physician or nurse, to report the adverse reaction.
Following notification, I would follow established protocols for managing adverse reactions, which might include administering emergency medications (if trained and authorized), providing supportive care, and documenting the event thoroughly. Accurate and timely documentation is crucial for understanding the reaction and preventing similar incidents in the future. I would also stay with the patient, offering reassurance and continued monitoring until the medical team arrives and takes over.
Pharmacy Technician MCQ
Which of the following DEA forms is used to order Schedule II controlled substances?
options:
Which of the following is the MOST appropriate storage condition for unopened vials of insulin?
A prescription is written for Timolol 0.5% eye drops, 1 drop in both eyes twice daily. The bottle contains 5 mL. Approximately how many days will the bottle last, given that 20 drops equal 1 mL?
options:
A prescription is written for amoxicillin 250mg/5mL, dispense 150mL, Sig: 2.5mL PO TID for 10 days. What is the total quantity of amoxicillin, in milligrams, the patient will take over the course of the treatment?
A doctor prescribes a fentanyl patch for a patient experiencing chronic pain. Which of the following routes of administration is used for a fentanyl patch?
Options:
According to federal law, what is the maximum number of refills permitted for a prescription of a Schedule III controlled substance?
What is the recommended temperature range for storing vaccines in a refrigerator?
Options:
A patient presents a prescription for Zithromax. Which of the following is the generic name for this medication?
Options:
Which DEA form is used to report the theft or significant loss of controlled substances?
Which of the following is the brand name for loratadine?
A physician orders 1 liter of D5W to be infused over 8 hours. The drop factor is 15 drops/mL. What is the correct flow rate in drops per minute?
A patient is prescribed prednisone 10 mg twice daily and 5 mg once daily. What is the total daily dose of prednisone the patient is receiving?
options:
According to the Poison Prevention Packaging Act (PPPA), which of the following medications must be dispensed in a child-resistant container?
options:
A pharmacist receives a prescription for amoxicillin suspension. Which of the following auxiliary labels is MOST appropriate to affix to the dispensed medication?
options:
A patient is 5'8" tall and weighs 180 pounds. What is their Body Mass Index (BMI)?
options:
A prescription is received with the notation 'DAW 1' written on it. What does this instruction mean to the pharmacy technician?
options:
A prescription is written with the abbreviation 'qs'. What does 'qs' mean in prescription terminology?
options:
A pharmacy needs to dispose of expired controlled substances. Which of the following is the MOST appropriate method for disposal?
options:
A patient presents a prescription for a fungal infection. Which of the following medications is MOST likely prescribed to treat this condition?
Options:
Lisinopril belongs to which of the following drug classes?
Options:
A customer wants to purchase two packages of pseudoephedrine, each containing 3.6 grams of pseudoephedrine. What is the total amount of pseudoephedrine, in milligrams, that the customer is attempting to purchase?
A physician prescribes nystatin suspension for a patient with oral thrush. Which of the following is the MOST appropriate route of administration?
options:
A pharmacy technician is preparing to compound a prescription. Which of the following is the MOST appropriate use for a Class III torsion balance?
options:
A pharmacy technician receives a prescription but the pharmacist on duty is on their lunch break and unavailable to verify the prescription. What is the MOST appropriate course of action?
Which of the following is the MOST appropriate use for a graduated cylinder in a pharmacy setting?
Options:
Which Pharmacy Technician skills should you evaluate during the interview phase?
While a single interview can't fully capture a candidate's abilities, focusing on core competencies is key. For Pharmacy Technicians, certain skills are more predictive of success than others. Let's explore which skills you should prioritize evaluating during the interview phase.
Pharmaceutical Knowledge
Assessing pharmaceutical knowledge can be streamlined with relevant MCQs. Our technical aptitude test includes questions to filter candidates who have a good grasp of the basics.
To further assess a candidate's knowledge, pose targeted interview questions. This will help you understand the depth of their understanding.
Describe the difference between a generic drug and a brand-name drug, and why this distinction matters to patients and pharmacies.
Look for candidates who can clearly articulate the differences, including cost implications and bioequivalence. Their answer should show an understanding of the importance of both types of medications.
Attention to Detail
You can use an assessment to quickly filter out for attention to detail. Adaface's attention to detail test screens for candidates who can spot errors and inconsistencies.
Directly assess this skill by presenting a scenario that requires careful analysis. These questions will reveal if they can find the small details.
Imagine you are preparing a prescription and notice the dosage is unusually high. What steps would you take?
The ideal candidate will explain they would double-check the prescription with the pharmacist and verify the dosage with the prescribing doctor. They should also understand the significance of questioning unusual prescriptions.
Communication Skills
Assess a candidate's communication abilities with an assessment. Our communication test will filter candidates who have good interpersonal skills.
Explore their communication style with targeted questions. Focus on how they handle interactions with patients and colleagues.
Describe a time you had to explain a complex medication instruction to a patient who was struggling to understand. How did you ensure they understood the information?
Listen for responses that emphasize empathy, clear explanations, and checking for understanding. The candidate should show that they can adapt their communication style to meet the patient's needs.
3 Tips for Maximizing Your Pharmacy Technician Interview Process
Before you put these Pharmacy Technician interview questions to use, here are a few tips to help you get the most out of your interview process. These tips will help you effectively assess candidates and make informed hiring decisions.
1. Leverage Skills Assessments to Streamline Candidate Screening
Skills assessments are an invaluable tool for quickly and objectively evaluating a candidate's technical abilities. This allows you to focus your interview time on candidates who demonstrate the core competencies needed for the role.
Consider using a Pharmacy Technician Test to gauge their knowledge of pharmaceutical calculations, drug identification, and dosage dispensing. For roles requiring computer skills, a Basic Computer Skills Test or Computer Literacy Test can be beneficial.
By using skills tests, you can efficiently filter out candidates who lack the necessary skills, saving time and resources in the long run. This approach ensures that you're only interviewing candidates who have a strong chance of succeeding in the role. Adaface's test library provides role specific tests to streamline the process.
2. Strategically Outline Your Interview Questions
Time is limited during interviews, so it's important to select a focused set of questions that reveal critical information. Choosing the right questions helps you evaluate candidates on the most important aspects of the role.
Consider questions related to customer service, problem-solving, and attention to detail. Explore questions related to communication skills to see how well the candidate can convey information. Also, there are many other types of interview questions that can be used too.
You can also use situational judgement interview questions to assess how they would handle the common scenarios in a pharmacy setting.
3. Master the Art of the Follow-Up Question
Simply asking a question isn't always enough to get a complete picture of a candidate's abilities. Follow-up questions help you uncover the true depth of their knowledge and experience.
For example, if a candidate describes their experience with a particular medication, ask a follow-up question like, "Can you describe a time when you had to make an important dosage adjustment for this medication, and what factors did you consider?" This will help you assess their decision-making process and level of expertise.
Hire Pharmacy Technicians with Confidence: Skills Tests and Interviews
Looking to hire Pharmacy Technicians with the right skills? Accurately assessing their abilities is key to making the right hire. Using skills tests, like the Pharmacy Technician Test, is the most efficient and accurate way to evaluate candidates.
Once you've identified top candidates with skills tests, you can confidently move them forward to the interview stage. Sign up for a free trial on our assessment platform to streamline your hiring process.
Pharmacy Technician Test
Download Pharmacy Technician interview questions template in multiple formats
Pharmacy Technician Interview Questions FAQs
Basic questions cover topics like medication knowledge, customer service skills, and adherence to pharmacy procedures.
Intermediate questions explore experience with inventory management, insurance processing, and handling prescription refills.
Advanced questions assess knowledge of compounding, sterile product preparation, and regulatory compliance.
Expert questions evaluate experience with specialized pharmacy software, managing complex patient cases, and leading pharmacy teams.
Focus on assessing technical knowledge, attention to detail, customer service aptitude, and problem-solving capabilities.
Use a combination of behavioral, situational, and technical questions to evaluate candidates thoroughly. Also, consider skills tests to assess practical abilities.

40 min skill tests.
No trick questions.
Accurate shortlisting.
We make it easy for you to find the best candidates in your pipeline with a 40 min skills test.
Try for freeRelated posts
Free resources