Hiring a pharmacist requires more than just verifying their credentials; it demands a thorough assessment of their knowledge, skills, and suitability for the role, much like when you are hiring an HR manager. A well-prepared interview questions list ensures you cover all bases.
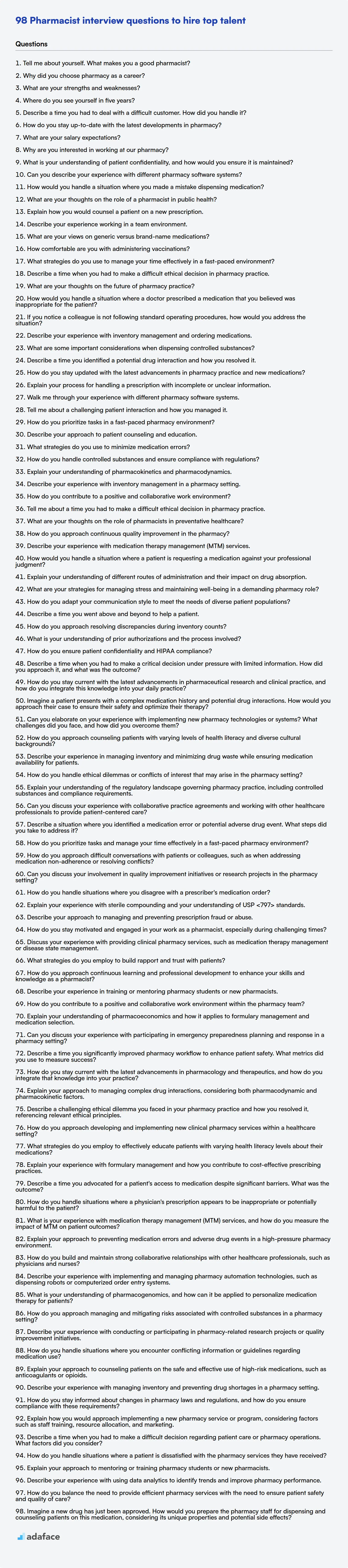
This blog post provides a list of pharmacist interview questions categorized by difficulty level, from basic to expert, along with multiple-choice questions to assess their knowledge effectively. It is designed to guide recruiters and hiring managers in evaluating candidates for pharmacy positions.
By using these questions, you'll be able to identify top talent and make informed hiring decisions, and for a standardized, objective assessment, consider using a pharmacist test or a pharmacy technician test before the interview.
Table of contents
Basic Pharmacist interview questions
1. Tell me about yourself. What makes you a good pharmacist?
I am a highly motivated and detail-oriented pharmacist with a strong foundation in pharmaceutical sciences and patient care. I excel at accurately dispensing medications, providing comprehensive drug information, and collaborating with healthcare teams to optimize patient outcomes. I am adept at identifying and resolving medication-related issues, ensuring patient safety and adherence. I'm passionate about staying current with the latest advancements in pharmacy practice and using my knowledge to improve the health and well-being of my patients.
What makes me a good pharmacist is a combination of factors. I possess strong clinical knowledge and critical thinking skills, enabling me to make informed decisions regarding medication therapy. I am also a skilled communicator, capable of effectively counseling patients and collaborating with other healthcare professionals. Furthermore, I am deeply committed to providing compassionate and patient-centered care, ensuring that each patient feels valued and supported. My ability to learn quickly and adapt to new situations also allows me to be effective in any pharmacy setting.
2. Why did you choose pharmacy as a career?
I chose pharmacy because I've always been fascinated by the intersection of science and healthcare, particularly how medications can improve people's lives. I enjoy problem-solving and the detail-oriented nature of the work, and pharmacy offers the chance to directly impact patient well-being through medication management and counseling. I also appreciate the continuous learning involved in staying updated on new drugs and therapies.
Furthermore, I was drawn to the various career paths within pharmacy, from community practice to hospital pharmacy and research. This provides flexibility and opportunities for professional growth as I progress in my career.
3. What are your strengths and weaknesses?
My strengths include my problem-solving abilities, adaptability, and strong communication skills. I'm also a quick learner and enjoy collaborating with others. For example, when faced with a complex bug during my last project, I was able to effectively debug the code, using print statements and debugger tools, and communicate the fix to the team, resulting in a timely resolution.
As for weaknesses, I sometimes struggle with delegating tasks, as I tend to want to ensure everything is done to a specific standard. I am actively working on improving this by trusting my team members and providing clear instructions and support when needed. I also recognize that I can sometimes get caught up in the details and lose sight of the bigger picture. I'm addressing this by regularly stepping back and assessing the overall progress and goals of a project.
4. Where do you see yourself in five years?
In five years, I envision myself as a senior [Your Job Title], deeply involved in [Specific area of interest related to the job or company]. I aim to have expanded my expertise in [mention 1-2 specific technologies or skills] and be contributing significantly to [Company/Team Goal].
Specifically, I hope to be leading projects in [mention specific project type or domain], mentoring junior team members, and consistently delivering innovative solutions that drive [positive business outcome]. I am eager to grow with the company and become a valuable asset, while continually learning and adapting to the evolving technological landscape. Example: Leading projects in cloud infrastructure automation, mentoring junior team members, and consistently delivering innovative solutions that drive cost efficiency.
5. Describe a time you had to deal with a difficult customer. How did you handle it?
In a previous role at a software company, I encountered a client who was consistently frustrated with the implementation of a new feature. They felt it wasn't meeting their specific business needs despite our initial agreements. I started by actively listening to their concerns, patiently letting them express their frustrations without interruption. I then summarized their issues to ensure I understood them correctly and acknowledged the impact on their workflow.
Next, I worked with our technical team to identify potential solutions and workarounds that could address their core problems. I presented these options to the client, clearly explaining the pros and cons of each. Eventually, we implemented a customized solution that, while not originally planned, significantly improved their experience. The key was empathy, clear communication, and a willingness to be flexible and find creative solutions to resolve their issue. This turned a potentially negative interaction into a stronger client relationship.
6. How do you stay up-to-date with the latest developments in pharmacy?
I stay current with pharmacy advancements through a combination of resources. I regularly read professional journals like the Journal of the American Pharmacists Association and Pharmacotherapy. I also subscribe to newsletters and email updates from organizations such as the FDA and ASHP to stay informed about new drug approvals, safety alerts, and regulatory changes.
Furthermore, I attend continuing education (CE) events, both online and in-person at conferences, to learn about emerging therapies, practice guidelines, and technological innovations. I also engage with professional networks and online forums to discuss recent findings and best practices with peers. Finally, I utilize resources like PubMed and other scientific databases for research purposes as needed.
7. What are your salary expectations?
My salary expectations are in line with the market rate for a [Job Title] with [Number] years of experience in [Relevant Skills/Industry] in the [Location] area. Based on my research, a reasonable range would be between $[Lower Bound] and $[Upper Bound] annually.
However, I am open to discussing this further based on the specifics of the role, the overall compensation package including benefits, and the opportunities for growth within the company. I'm more focused on finding the right fit and a challenging opportunity where I can contribute significantly to the team.
8. Why are you interested in working at our pharmacy?
I'm interested in working at your pharmacy because I'm impressed by your commitment to patient care and community involvement. I've heard positive things about your pharmacy's reputation for providing personalized service and building strong relationships with customers, which aligns with my own values as a pharmacy professional.
Furthermore, I am looking for a pharmacy that prioritizes innovation and continuous improvement. Your pharmacy's forward-thinking approach is something I admire, and I believe I can contribute my skills and experience to further enhance your pharmacy's success. The opportunity to learn from experienced pharmacists and contribute to a positive and supportive work environment is also very appealing.
9. What is your understanding of patient confidentiality, and how would you ensure it is maintained?
Patient confidentiality, often protected by laws like HIPAA, means protecting a patient's personal and health information from unauthorized disclosure. My understanding is that all information related to a patient's care, including their identity, medical history, treatment plans, and even appointment schedules, is private and should only be shared with individuals directly involved in their care or when legally required.
To ensure patient confidentiality, I would adhere to the following practices: always discussing patient information in private settings, using secure communication channels for electronic data, properly disposing of sensitive documents, strictly following organizational policies on data access and sharing, obtaining proper consent before releasing information, and being vigilant about potential breaches of privacy. Regular training and awareness of ethical considerations regarding patient data is also crucial.
10. Can you describe your experience with different pharmacy software systems?
I have experience with a few different pharmacy software systems. I've used QS/1, which I found user-friendly for prescription processing and inventory management. I also have experience with PioneerRx, where I focused on using its reporting features to track key performance indicators like days-to-fill and inventory turnover. In addition to these, I've worked with EnterpriseRx, primarily for its comprehensive patient profile management and third-party billing capabilities.
My experience involves tasks such as prescription entry and verification, insurance adjudication, inventory control, and generating reports. I am comfortable learning new systems and adapting to different workflows. I'm familiar with the common functions needed for retail pharmacy operations.
11. How would you handle a situation where you made a mistake dispensing medication?
If I made a medication dispensing error, my immediate priority would be patient safety. I would promptly assess the patient for any adverse effects and provide necessary interventions. I would then immediately report the error to the supervising pharmacist or physician, providing a detailed account of what happened, including the medication, dosage, route, and time of administration, as well as the potential impact on the patient.
Following the immediate response, I would thoroughly document the incident according to established procedures. This includes completing an incident report and participating in any investigations to identify the root cause of the error. I would actively seek opportunities to learn from the mistake, such as reviewing relevant protocols, seeking clarification on any unclear aspects, and participating in training programs to prevent similar errors in the future. Finally, I would communicate honestly and empathetically with the patient (or their family) about the error, as directed by the pharmacist or physician, ensuring they are informed and supported throughout the process. Open communication is key to maintain trust and ensure the patient receives the best possible care.
12. What are your thoughts on the role of a pharmacist in public health?
Pharmacists play a crucial role in public health, extending beyond dispensing medications. They are accessible healthcare professionals who can contribute significantly to disease prevention, health promotion, and chronic disease management. Their responsibilities include administering vaccinations, providing medication therapy management, educating patients on proper medication use and adherence, and participating in public health campaigns related to smoking cessation, diabetes prevention, and opioid overdose prevention.
Furthermore, pharmacists can assist in disease surveillance and reporting, identifying trends in medication use and potential outbreaks. They can also work in collaboration with other healthcare providers and community organizations to address public health challenges and improve health outcomes for underserved populations. By leveraging their expertise and accessibility, pharmacists are valuable assets in promoting a healthier community.
13. Explain how you would counsel a patient on a new prescription.
When counseling a patient on a new prescription, I would first introduce myself and verify the patient's identity and any known allergies. Then, I would explain the name of the medication, what condition it treats, and how it works in simple terms. I'd also cover the correct dosage, frequency, and route of administration, and when they should expect to see improvement.
I would also discuss potential side effects, including common and serious ones, and what actions to take if they occur. Crucially, I'd review any food or drug interactions, and answer all their questions. I would also confirm they know how to store the medicine and when to seek medical attention. Finally, I would double check their understanding and offer them an opportunity to ask any final questions.
14. Describe your experience working in a team environment.
I thrive in collaborative team environments. I believe effective communication, mutual respect, and a shared understanding of goals are crucial for success. In my previous role, I actively participated in daily stand-up meetings, providing updates on my progress and identifying any roadblocks I encountered. I also proactively offered assistance to teammates when needed, fostering a supportive and collaborative atmosphere. For instance, when a colleague was struggling with a particularly challenging bug, I paired with them, sharing my debugging techniques and helping them identify the root cause, which significantly sped up the resolution process.
Furthermore, I'm comfortable with various collaboration tools and methodologies such as Agile and Scrum. I actively engage in code reviews, providing constructive feedback and learning from others. I believe that teamwork multiplies our individual strengths, leading to better outcomes than any one person could achieve alone. My focus is always on contributing positively to the team's overall success, whether by sharing my expertise or learning from others.
15. What are your views on generic versus brand-name medications?
Generic and brand-name medications contain the same active ingredients and are held to the same FDA standards regarding safety, effectiveness, and manufacturing quality. Generics are typically significantly cheaper because the manufacturers don't have to recoup the initial research and development costs. The inactive ingredients may vary, but these are not supposed to affect the drug's performance.
My view is that generic medications are a safe and cost-effective alternative for most people. However, certain individuals might experience different results due to variations in inactive ingredients, especially in drugs with narrow therapeutic windows (where small changes in dosage can have significant effects). In such cases, consultation with a doctor or pharmacist is important.
16. How comfortable are you with administering vaccinations?
I am comfortable with administering vaccinations, although my experience varies depending on the specific type of vaccine and the target population. I have experience with intramuscular and subcutaneous injections, including proper technique for site selection, needle gauge, and administration. I am also familiar with vaccine storage protocols, documentation procedures, and managing potential adverse reactions.
To ensure I am fully competent with any specific vaccine or protocol, I always review relevant guidelines and receive appropriate training before administering a new vaccine. I am also comfortable using electronic health record systems to document vaccinations and track patient information.
17. What strategies do you use to manage your time effectively in a fast-paced environment?
In fast-paced environments, I prioritize tasks ruthlessly using methods like the Eisenhower Matrix (urgent/important). I create a daily to-do list, focusing on the most impactful items first, and block out specific time slots in my calendar for focused work. I minimize distractions by turning off notifications and communicating my availability to colleagues.
To stay organized, I use tools like task management apps and note-taking software. Regularly reviewing my progress and adjusting priorities throughout the day is crucial. Also, I delegate tasks when appropriate and don't hesitate to ask for help if I'm feeling overwhelmed. I try to Batch similar tasks together to improve efficiency.
18. Describe a time when you had to make a difficult ethical decision in pharmacy practice.
During my pharmacy internship, I encountered a situation where a patient frequently requested early refills for their opioid pain medication. While the patient claimed to have lost their medication or had it stolen on several occasions, the frequency raised concerns about potential misuse or diversion. I had to weigh the patient's right to pain management against my ethical obligation to prevent drug abuse and ensure patient safety. After consulting with the supervising pharmacist, we decided to counsel the patient on responsible medication use and explore alternative pain management strategies with their physician. We also implemented stricter monitoring of their refills and communicated our concerns to the prescriber.
This decision was difficult because I wanted to help alleviate the patient's pain, but I also recognized the potential harm associated with opioid misuse. By collaborating with the pharmacist and physician, we were able to address the ethical dilemma in a way that prioritized the patient's well-being while minimizing the risk of drug abuse. It highlighted the importance of professional judgment, communication, and adherence to ethical guidelines in pharmacy practice.
19. What are your thoughts on the future of pharmacy practice?
The future of pharmacy practice is evolving rapidly, driven by technology, changing healthcare models, and increasing patient needs. I believe pharmacists will play a more significant role in preventative care, chronic disease management, and personalized medicine. Telepharmacy and digital health solutions will expand access to care, especially in underserved areas.
Pharmacists will likely have greater prescribing authority and collaborate more closely with physicians and other healthcare providers as part of integrated care teams. Automation and artificial intelligence will handle routine tasks like dispensing, allowing pharmacists to focus on patient counseling, medication therapy management, and complex clinical decision-making. Continuing education and specialization will be crucial for pharmacists to stay current with advancements in pharmacology and therapeutics.
20. How would you handle a situation where a doctor prescribed a medication that you believed was inappropriate for the patient?
If I believed a prescribed medication was inappropriate, my first step would be to privately and respectfully discuss my concerns with the prescribing doctor. I would present my rationale, including any relevant information such as the patient's history, potential drug interactions, or evidence-based guidelines. It's crucial to maintain a collaborative and professional approach, recognizing the doctor's expertise and the potential for differing clinical judgment.
If, after discussing my concerns, I still believed the medication was inappropriate and potentially harmful, I would escalate the issue through the appropriate channels, following the established protocols within my organization or healthcare system. This might involve consulting with a senior colleague, a pharmacist, or the medical director. My priority would always be the patient's safety and well-being, while upholding ethical and professional standards.
21. If you notice a colleague is not following standard operating procedures, how would you address the situation?
If I noticed a colleague not following standard operating procedures, I would first try to understand the reason behind their deviation. I would approach them privately and ask if they are facing any challenges or if they are aware of the correct procedure. Perhaps they are unaware of a recent update, or they're encountering a specific obstacle that prevents them from following the standard.
Depending on the reason, I would offer assistance or clarification. If it's a matter of lacking knowledge, I'd point them to the relevant documentation or offer to walk them through the process. If the reason is due to some impediment, I will either help solve the issue if I can or escalate it to the appropriate channels (e.g., supervisor or team lead) to ensure consistent adherence to procedures and to maintain quality standards.
22. Describe your experience with inventory management and ordering medications.
In my previous role, I was responsible for managing the pharmacy's inventory, which included ordering and stocking medications. I utilized inventory management software to track stock levels, monitor expiration dates, and forecast demand. This helped prevent stockouts and minimize waste.
My experience also includes placing orders with pharmaceutical wholesalers, negotiating pricing, and ensuring compliance with controlled substance regulations. I'm familiar with various inventory control methods, such as FIFO (First-In, First-Out), and I'm adept at reconciling invoices and resolving discrepancies with suppliers.
23. What are some important considerations when dispensing controlled substances?
When dispensing controlled substances, several critical considerations are paramount. First, verifying the prescription's legitimacy is crucial. This includes confirming the prescriber's DEA number, ensuring the prescription falls within their scope of practice, and scrutinizing for any signs of alteration or forgery. Patient identification must also be verified to prevent diversion. Accurate record-keeping is essential, including maintaining a perpetual inventory of controlled substances and documenting all dispensing activities.
Furthermore, understanding state and federal regulations related to controlled substance dispensing is vital. This includes quantity limits, refill restrictions, and reporting requirements to prescription drug monitoring programs (PDMPs). Pharmacists should be vigilant for red flags, such as patients paying in cash or requesting early refills, and use their professional judgment to determine whether dispensing is appropriate. Proper storage and security of controlled substances are also necessary to prevent theft and diversion.
Intermediate Pharmacist interview questions
1. Describe a time you identified a potential drug interaction and how you resolved it.
During a clinical rotation, I noticed a patient was prescribed warfarin and a newly prescribed antibiotic, clarithromycin. Recognizing clarithromycin's potential to inhibit CYP3A4, a key enzyme in warfarin metabolism, I anticipated a potential increase in the patient's INR and risk of bleeding. I consulted with the attending physician and pharmacist.
We decided to closely monitor the patient's INR more frequently during the antibiotic course. The pharmacist recommended a temporary reduction in the warfarin dosage based on the severity of interaction and patient factors. The INR was indeed elevated initially, but with the adjusted warfarin dose and close monitoring, we successfully navigated the interaction without any adverse events, eventually returning the patient to their original warfarin dose after the antibiotic course.
2. How do you stay updated with the latest advancements in pharmacy practice and new medications?
I stay updated through a variety of methods including: regularly reading professional pharmacy journals like the Journal of the American Pharmacists Association and Pharmacotherapy, subscribing to newsletters from organizations like the FDA and ASHP, and participating in continuing education (CE) programs and webinars. I also attend pharmacy conferences and workshops to learn about new research, guidelines, and best practices directly from experts.
Furthermore, I utilize online resources such as Medscape, PubMed, and reputable drug information databases to research specific medications and therapeutic areas. Networking with colleagues and participating in professional online forums are also valuable ways to stay informed about real-world experiences and emerging trends in pharmacy.
3. Explain your process for handling a prescription with incomplete or unclear information.
When I encounter a prescription with incomplete or unclear information, my first step is to attempt to clarify the missing details. This often involves directly contacting the prescribing physician or their office. I would use professional communication, clearly stating the missing or ambiguous information and requesting the necessary clarification to ensure patient safety and accurate dispensing.
If I'm unable to reach the prescriber immediately, I would document my attempts and consult with a senior pharmacist or my supervisor for guidance. We might consider alternative methods for obtaining the information, such as checking the patient's profile for previously prescribed medications or contacting the patient directly for relevant details, always ensuring compliance with HIPAA regulations. Patient safety is paramount, and I would never dispense a medication without confirming the necessary information.
4. Walk me through your experience with different pharmacy software systems.
Throughout my career, I've gained experience with several pharmacy software systems. I am proficient in using Rx30 and PioneerRx for prescription processing, inventory management, and patient profile maintenance. My experience includes data entry, claims adjudication, report generation, and resolving common system errors.
Additionally, I've worked with ancillary systems like QS/1 for specialized compounding needs and have integrated with various Electronic Health Record (EHR) systems for data exchange and improved patient care coordination. I'm comfortable learning new software and adapting to different system functionalities quickly.
5. Tell me about a challenging patient interaction and how you managed it.
In a previous role, I encountered a patient who was consistently non-compliant with their medication regimen and became agitated during appointments. They felt the medication was not effective and expressed frustration with the perceived lack of progress. I actively listened to their concerns, validated their feelings, and worked to establish a rapport by acknowledging the difficulties they were experiencing.
I then collaborated with the patient and the physician to explore alternative medication options and lifestyle adjustments. By involving the patient in the decision-making process and providing clear explanations about the rationale behind the changes, we were able to improve their adherence and reduce their agitation, ultimately leading to a more positive outcome. It was crucial to remain patient, empathetic, and collaborative throughout the process.
6. How do you prioritize tasks in a fast-paced pharmacy environment?
In a fast-paced pharmacy, prioritization is crucial. I would first assess each task based on urgency and importance. Patient safety is always the top priority, so filling prescriptions, addressing immediate patient needs (counseling, resolving drug interactions), and handling urgent requests from doctors would come first. Then, I'd tackle other essential tasks, such as inventory management and insurance claims, based on deadlines and potential impact on pharmacy operations.
To stay organized, I would use a combination of techniques: a running to-do list, clear communication with the team to delegate tasks when possible, and a quick reassessment of priorities whenever new tasks arise. I'd also be proactive in identifying potential bottlenecks and finding ways to streamline workflows to improve efficiency.
7. Describe your approach to patient counseling and education.
My approach to patient counseling and education centers on empathy and clear communication. I start by actively listening to the patient's concerns and understanding their current knowledge level. Then, I tailor my explanation of their condition, treatment plan, or medication to their specific needs, using plain language and avoiding jargon. I encourage questions and provide resources like written materials or reliable websites to reinforce their understanding.
I also emphasize the importance of adherence to the treatment plan and discuss potential side effects and how to manage them. My goal is to empower patients to take an active role in their health by providing them with the knowledge and support they need to make informed decisions. I check for understanding by asking the patient to explain back to me the key details discussed.
8. What strategies do you use to minimize medication errors?
To minimize medication errors, I prioritize thoroughness and verification at each step of the medication process. I always double-check the medication name, dosage, route, and timing against the physician's order and the patient's medical record. Utilizing available technology like barcode scanners helps ensure the right medication is selected and reduces the risk of look-alike, sound-alike medication errors. Furthermore, I actively engage with patients to confirm their understanding of the medication and address any concerns they might have regarding allergies or existing medications.
I also believe in a culture of open communication and collaboration. If I have any doubts or discrepancies, I immediately clarify them with the prescribing physician or pharmacist. I proactively report any errors or near misses to contribute to learning and improvement within the healthcare team. Participating in medication safety training and staying updated on best practices are also crucial to minimizing errors.
9. How do you handle controlled substances and ensure compliance with regulations?
Handling controlled substances requires strict adherence to federal and state regulations. This includes maintaining accurate records of receipt, storage, dispensing, and disposal. Key practices involve using a double-lock system for storage, conducting regular inventory audits to reconcile quantities, and promptly reporting any discrepancies or losses to the relevant authorities (e.g., DEA).
Furthermore, all personnel involved in handling controlled substances must be properly trained and authorized. This training should cover proper handling procedures, record-keeping requirements, and security protocols. Proper disposal methods, as mandated by regulations, such as reverse distribution or destruction, are essential to prevent diversion and misuse.
10. Explain your understanding of pharmacokinetics and pharmacodynamics.
Pharmacokinetics (PK) describes what the body does to a drug, encompassing absorption, distribution, metabolism, and excretion (ADME). It focuses on how drug concentrations change over time in different parts of the body. Essentially, it's about how the body processes the drug.
Pharmacodynamics (PD), on the other hand, describes what the drug does to the body. It examines the relationship between drug concentration and its effect, including both desired therapeutic effects and unwanted side effects. It includes the mechanism of action and effects of drugs on cells, tissues, and the body.
11. Describe your experience with inventory management in a pharmacy setting.
In my pharmacy experience, I was responsible for maintaining optimal inventory levels to ensure patient needs were met while minimizing waste and costs. This involved regular monitoring of stock levels using pharmacy software (like RxInventory), ordering medications and supplies from wholesalers (e.g., McKesson), and conducting physical inventory counts.
Specifically, I managed inventory by tracking expiration dates, rotating stock (FIFO), and resolving discrepancies between physical and recorded inventory. I also participated in analyzing usage patterns to adjust ordering quantities and prevent stockouts of critical medications. This included monitoring PAR levels and implementing automated ordering systems where possible.
12. How do you contribute to a positive and collaborative work environment?
I actively contribute to a positive and collaborative work environment by practicing open and honest communication. I believe in sharing information proactively, actively listening to my colleagues' ideas and concerns, and providing constructive feedback in a respectful manner.
Furthermore, I am always willing to offer assistance to team members who may be struggling, whether it's helping debug code, sharing my knowledge, or simply providing a fresh perspective. I also make an effort to celebrate team successes and acknowledge individual contributions to foster a sense of camaraderie and shared accomplishment. I believe that a supportive and encouraging atmosphere leads to increased productivity and job satisfaction.
13. Tell me about a time you had to make a difficult ethical decision in pharmacy practice.
During my rotation at a community pharmacy, a patient presented a prescription for a high-dose opioid painkiller, and their behavior seemed erratic and suggestive of potential opioid abuse. The physician was known for being quite liberal with prescribing these medications. I had to decide whether to fill the prescription as written or to take action.
I consulted with the supervising pharmacist, and we decided to contact the prescribing physician to express our concerns and inquire about the patient's history and current treatment plan. The physician appreciated the concern, re-evaluated the patient, and ultimately adjusted the prescription to a lower dose and added a referral to a pain management specialist. This ensured the patient received appropriate care while mitigating the potential for abuse, aligning with my ethical responsibility to prioritize patient well-being and safety.
14. What are your thoughts on the role of pharmacists in preventative healthcare?
Pharmacists are uniquely positioned to play a significant role in preventative healthcare. Their accessibility within communities makes them ideal points of contact for patient education, screening, and vaccinations. They can provide valuable counseling on topics like medication adherence, lifestyle modifications, and disease prevention strategies.
Specifically, pharmacists can contribute by administering immunizations (e.g., flu shots, shingles vaccines), conducting screenings for conditions like diabetes and hypertension, and offering medication therapy management to optimize drug regimens and reduce adverse effects. Their expertise in medications allows them to identify potential drug interactions and counsel patients on how to manage their medications safely and effectively, promoting better health outcomes and preventing hospitalizations.
15. How do you approach continuous quality improvement in the pharmacy?
Continuous quality improvement (CQI) in a pharmacy involves a systematic approach to enhance services and patient outcomes. Key steps include:
- Identify areas for improvement: This involves analyzing data (e.g., medication errors, patient satisfaction surveys), gathering feedback from staff, and observing workflows.
- Develop and implement interventions: Based on identified areas, create action plans with specific goals, assign responsibilities, and set timelines. Interventions might include process changes, staff training, or new technology implementation.
- Monitor and evaluate: Track the effectiveness of interventions using relevant metrics. Data analysis helps determine if the changes are leading to desired improvements. Make adjustments as needed based on findings, ensuring a cycle of continuous refinement and optimal patient care.
16. Describe your experience with medication therapy management (MTM) services.
My experience with Medication Therapy Management (MTM) services includes providing comprehensive medication reviews (CMRs) and targeted medication reviews (TMRs) to patients with chronic conditions. I've worked to identify and resolve medication-related problems, such as drug interactions, adverse effects, and adherence issues. This often involved collaborating with physicians and other healthcare providers to optimize medication regimens and improve patient outcomes.
I have experience documenting MTM encounters, submitting claims for services rendered, and using various software platforms to manage patient information and track outcomes. Additionally, I'm familiar with the core elements of an MTM program, including patient enrollment, data collection, intervention, and evaluation.
17. How would you handle a situation where a patient is requesting a medication against your professional judgment?
If a patient requests medication that I believe is not in their best interest or could be harmful, I would first explain my concerns clearly and empathetically. I would discuss the potential risks and side effects of the medication, as well as alternative treatment options that might be more appropriate given their condition.
I would document the patient's request, my professional judgment, and the rationale behind my decision. If the patient remains insistent, I would explore seeking a second opinion from a colleague or consulting with a supervising physician, always prioritizing the patient's well-being while respecting their autonomy to the extent possible within ethical and legal boundaries. If, after exhausting all reasonable options, the patient still demands the medication and I firmly believe it would be detrimental, I would refuse to prescribe it, explaining that my primary duty is to do no harm.
18. Explain your understanding of different routes of administration and their impact on drug absorption.
Routes of administration significantly impact drug absorption. Intravenous (IV) administration bypasses absorption altogether, resulting in 100% bioavailability. Oral administration involves absorption from the gastrointestinal tract, which can be affected by factors such as pH, food, and first-pass metabolism, leading to variable bioavailability. Subcutaneous (SC) and intramuscular (IM) routes offer relatively slower absorption compared to IV but faster than oral, with absorption rates influenced by blood flow at the injection site. Other routes like sublingual (under the tongue) and transdermal (across the skin) provide direct entry into the bloodstream, avoiding first-pass metabolism, but absorption rates can vary based on the drug's properties and individual physiology.
Different routes have varying onset and duration of action. IV administration leads to rapid onset and precise control of drug concentration, while oral and transdermal routes provide a more sustained but less predictable effect. Understanding these differences is crucial for selecting the appropriate route to achieve the desired therapeutic outcome.
19. What are your strategies for managing stress and maintaining well-being in a demanding pharmacy role?
In a demanding pharmacy role, I prioritize strategies that promote both stress management and overall well-being. I focus on time management by prioritizing tasks, delegating when appropriate, and setting realistic deadlines to avoid feeling overwhelmed. Outside of work, I engage in activities that help me de-stress, such as regular exercise, spending time in nature, and pursuing hobbies. I also maintain a strong support system of friends and family, and I'm not afraid to ask for help when needed.
Moreover, I practice mindfulness and meditation techniques to stay grounded and focused in the present moment, which helps reduce anxiety and improve resilience. I am also committed to continuous professional development. This not only expands my skill set, but also increases my confidence and job satisfaction, further contributing to my overall well-being. Ensuring I get adequate sleep and maintain a healthy diet is also crucial for managing stress and maintaining energy levels.
20. How do you adapt your communication style to meet the needs of diverse patient populations?
I adapt my communication by considering factors like cultural background, language proficiency, health literacy, and age. I use clear, simple language, avoiding jargon, and speak slowly when needed. I also actively listen to understand their perspective and concerns, using open-ended questions to encourage them to share information.
Furthermore, I utilize resources like professional interpreters or translated materials when language barriers exist. I'm mindful of non-verbal cues and cultural norms that might influence communication and always strive to create a comfortable and respectful environment. This includes being aware of different health beliefs and adapting explanations to align with their understanding.
21. Describe a time you went above and beyond to help a patient.
During my time as a medical assistant, I encountered a patient, Mrs. Davis, who was extremely anxious about an upcoming biopsy. Beyond explaining the procedure, I noticed she was worried about transportation and being alone afterward. To alleviate her concerns, I contacted our volunteer transport service and arranged a ride for her.
Knowing she lived alone, I also prepared a small care package with easy-to-eat snacks and a calming tea. After her biopsy, I called her to check in and ensure she was comfortable. She was incredibly grateful for the extra support, which eased her anxiety and made the whole process significantly less stressful for her.
22. How do you approach resolving discrepancies during inventory counts?
When discrepancies occur during inventory counts, my initial step is to re-count the item(s) in question, ensuring accuracy in my own count. If the discrepancy persists, I investigate potential causes such as misplaced items, errors in receiving or shipping records, data entry mistakes, or possible theft or damage. I would then compare the physical count to the system records, paying close attention to recent transactions and movement history.
If the source of the discrepancy is identified, I would take corrective action, such as adjusting inventory levels in the system, updating records, and implementing preventative measures to avoid similar issues in the future. If the discrepancy remains unresolved, I escalate the issue to a supervisor or appropriate personnel, providing all relevant documentation and findings for further investigation.
23. What is your understanding of prior authorizations and the process involved?
Prior authorization is a requirement from a health insurance company that a healthcare provider must obtain approval before prescribing a specific medication, performing a procedure, or offering a service. It's essentially a way for the insurance company to ensure the treatment is medically necessary and cost-effective, according to their guidelines.
The process typically involves the provider submitting a request with supporting documentation justifying the need for the treatment. The insurance company reviews this information, sometimes requiring additional details or a peer-to-peer review. If approved, the service is covered; if denied, the patient may have to pay out-of-pocket or appeal the decision. The turnaround time for approvals can vary, and denials often require exploring alternative treatments or appealing the insurance company's decision.
24. How do you ensure patient confidentiality and HIPAA compliance?
I understand that patient confidentiality and HIPAA compliance are critical. I ensure this by adhering to established policies and procedures, including using secure communication methods for transmitting Protected Health Information (PHI) and storing data in HIPAA-compliant environments. I also strictly control access to PHI, only accessing information necessary for my specific role and tasks.
Furthermore, I am committed to ongoing training related to HIPAA regulations and data privacy best practices. If dealing with data, I implement data encryption and access controls. If I'm unsure about a situation, I always consult with a supervisor or compliance officer to ensure I'm adhering to HIPAA regulations.
Advanced Pharmacist interview questions
1. Describe a time when you had to make a critical decision under pressure with limited information. How did you approach it, and what was the outcome?
During a critical system outage at my previous company, I was the on-call engineer. The primary database server had failed, and we had limited real-time monitoring data available due to the outage itself. I had to decide whether to initiate a full failover to the backup database, which was potentially behind in replication and could result in some data loss, or attempt an immediate repair of the primary database, which carried the risk of prolonging the outage if unsuccessful.
I quickly gathered the available information: the last known replication time, the estimated time to repair the primary server based on similar past incidents, and the impact of potential data loss versus prolonged downtime on our customers. I consulted with the senior database administrator remotely. Weighing the risks, I decided to initiate the failover. The outcome was a faster recovery, albeit with a small, acceptable amount of data loss. We communicated the data loss transparently to affected customers and worked to recover as much as possible from backups, minimizing the impact. This decision prevented a significantly longer outage and preserved the overall system integrity.
2. How do you stay current with the latest advancements in pharmaceutical research and clinical practice, and how do you integrate this knowledge into your daily practice?
I stay current through a multi-faceted approach. I regularly read leading peer-reviewed journals like The New England Journal of Medicine and The Lancet, as well as publications specific to my area of practice. I also actively participate in continuing medical education (CME) courses, attending conferences and webinars offered by professional organizations such as the American Pharmaceutical Association (APhA). Furthermore, I leverage online resources like PubMed and Medscape for research and updates on clinical trials and drug approvals.
Integrating this knowledge involves critically evaluating the evidence presented in these sources. I consider the study design, sample size, and potential biases before applying new findings to my practice. When appropriate, I discuss new information with colleagues to gain different perspectives and ensure a well-rounded understanding. I also update treatment protocols and patient education materials to reflect current best practices, ensuring patients receive the most up-to-date and evidence-based care. I always prioritize patient safety and tailor treatments to individual needs, weighing the potential benefits against the risks based on the latest available data.
3. Imagine a patient presents with a complex medication history and potential drug interactions. How would you approach their case to ensure their safety and optimize their therapy?
I would start by gathering a comprehensive medication history, including prescription drugs, over-the-counter medications, herbal supplements, and any allergies. I'd then use a reliable drug interaction database (like Lexicomp or Micromedex) to identify potential interactions, considering factors like dosage, route of administration, and patient-specific characteristics (age, renal/hepatic function, other comorbidities).
Next, I would assess the clinical significance of each potential interaction, differentiating between minor, moderate, and major risks. I'd collaborate with the patient's physician to develop a plan, which might include adjusting dosages, choosing alternative medications, closely monitoring for adverse effects, or discontinuing medications. Patient education is crucial; I would explain the risks and benefits of each medication and emphasize the importance of adherence and reporting any unusual symptoms. Finally, I would document all interventions and continue to monitor the patient's response to therapy.
4. Can you elaborate on your experience with implementing new pharmacy technologies or systems? What challenges did you face, and how did you overcome them?
In my previous role at [Pharmacy Name], I was involved in the implementation of a new automated dispensing system. A key challenge was the initial data migration and ensuring data integrity between the old and new systems. We addressed this by creating a detailed data mapping document and conducting thorough data validation checks at each stage of the migration. Another challenge was the staff training. Some pharmacists and technicians were initially resistant to change. We overcame this by providing comprehensive training sessions, including hands-on practice and ongoing support, which helped them become comfortable and confident with the new system.
Additionally, we faced some unexpected technical glitches during the initial rollout, such as intermittent connectivity issues with the medication database. To address these issues, we worked closely with the vendor's technical support team to troubleshoot and implement necessary software patches and hardware upgrades. We also established a clear communication channel with staff to keep them informed about the progress of the resolution and any temporary workarounds.
5. How do you approach counseling patients with varying levels of health literacy and diverse cultural backgrounds?
When counseling patients with varying health literacy, I prioritize clear and simple communication. I avoid jargon and use plain language, supplementing with visuals and teach-back methods to confirm understanding. For diverse cultural backgrounds, I adopt a culturally sensitive approach by researching cultural norms and beliefs related to health. I actively listen to the patient's perspective, acknowledge potential cultural differences, and adapt my communication style accordingly. Respect for their values and beliefs is paramount, and I may utilize interpreter services or culturally specific educational materials when necessary.
6. Describe your experience in managing inventory and minimizing drug waste while ensuring medication availability for patients.
In my previous role, I was responsible for overseeing inventory management to optimize stock levels and minimize drug waste. I implemented a First-Expired, First-Out (FEFO) system to ensure older medications were dispensed before newer ones, thereby reducing the likelihood of expiration. We also conducted regular inventory audits to identify slow-moving or expired medications, adjusting ordering quantities accordingly. I closely monitored usage patterns and collaborated with prescribers to anticipate demand fluctuations and ensure adequate medication availability for patients.
To further minimize waste, I worked to identify medications frequently wasted or partially used, such as topical ointments or inhalers. We educated staff and patients on proper administration techniques and emphasized the importance of using the full prescribed amount. Additionally, I explored opportunities to repackage medications into smaller, unit-dose formats to reduce waste and improve patient adherence.
7. How do you handle ethical dilemmas or conflicts of interest that may arise in the pharmacy setting?
When faced with ethical dilemmas or conflicts of interest in a pharmacy setting, my first step is to ensure patient safety and well-being. I would consult the relevant professional codes of ethics (e.g., from the American Pharmacists Association) and organizational policies to guide my decision-making. If unsure, I would discuss the situation with a trusted colleague, supervisor, or ethics committee to get different perspectives and ensure a well-reasoned approach.
My priority is always to act in the best interest of the patient while adhering to legal and ethical guidelines. This might involve disclosing the conflict of interest to the patient, seeking alternative treatment options, or recusing myself from the situation if necessary. Documentation of the dilemma and the actions taken is also crucial.
8. Explain your understanding of the regulatory landscape governing pharmacy practice, including controlled substances and compliance requirements.
My understanding of the regulatory landscape governing pharmacy practice encompasses federal and state laws, regulations, and guidelines designed to ensure patient safety and drug integrity. Key areas include the Controlled Substances Act (CSA), which dictates the handling, storage, and dispensing of controlled substances to prevent diversion and abuse. Compliance requirements involve accurate record-keeping, proper labeling, adherence to prescribing limits, and reporting suspicious activities.
Furthermore, state pharmacy laws and regulations govern licensure, scope of practice, and operational standards for pharmacies. I am familiar with the importance of maintaining up-to-date knowledge of these regulations, including USP <795>, <797> and <800> standards for compounding, HIPAA for patient privacy, and relevant fraud and abuse laws. Regular audits and inspections are essential to ensure ongoing compliance and prevent penalties.
9. Can you discuss your experience with collaborative practice agreements and working with other healthcare professionals to provide patient-centered care?
During my experience as a pharmacist, I've frequently worked under collaborative practice agreements (CPAs) to optimize patient care. These agreements outlined specific protocols and patient populations where I could independently manage medication therapy, order lab tests, and make dosage adjustments, all in coordination with the supervising physician. For example, I managed anticoagulation therapy for patients with atrial fibrillation under a CPA, regularly monitoring INR values, adjusting warfarin doses, and educating patients on their medication regimen.
Working collaboratively with physicians, nurses, and other healthcare professionals was essential. Regular communication, often through shared electronic health records or direct consultations, ensured everyone was informed and aligned on the patient's care plan. This team-based approach, facilitated by the CPA, improved patient outcomes, reduced hospital readmissions, and enhanced overall patient satisfaction.
10. Describe a situation where you identified a medication error or potential adverse drug event. What steps did you take to address it?
During a medication reconciliation, I noticed a patient was prescribed both warfarin and aspirin, without a clear indication or documented rationale for dual antiplatelet therapy. Recognizing the increased risk of bleeding, I immediately brought this to the attention of the attending physician.
I reviewed the patient's history, recent lab results (INR, platelet count), and current medications to gather supporting evidence. After discussing my concerns with the physician and providing the relevant data, we collaboratively decided to discontinue the aspirin and monitor the patient closely for any signs of bleeding. The change was documented in the patient's chart, and the patient was educated about the reason for the medication change and potential side effects to watch for.
11. How do you prioritize tasks and manage your time effectively in a fast-paced pharmacy environment?
In a fast-paced pharmacy, I prioritize tasks by immediately assessing urgency and importance. I use a mental or physical (if time permits) "Eisenhower Matrix" (Urgent/Important) to categorize tasks. Filling prescriptions accurately and dispensing medications to patients takes immediate priority, followed by addressing urgent requests from healthcare providers. Inventory management and other administrative tasks are handled as time allows, always keeping an eye on potential disruptions. I also communicate proactively with colleagues to redistribute workload or seek assistance when needed.
To manage time effectively, I use techniques like batching similar tasks (e.g., processing multiple refills at once), minimizing distractions, and leveraging available technology to automate repetitive processes. Clear communication and delegation are also key. I regularly reassess my priorities and adjust my schedule as new demands arise. Regularly checking in with my team to see if anyone requires help keeps our service levels up to par.
12. How do you approach difficult conversations with patients or colleagues, such as when addressing medication non-adherence or resolving conflicts?
When approaching difficult conversations, I prioritize empathy and active listening. I start by creating a safe and respectful environment where the other person feels comfortable sharing their perspective. I use open-ended questions to understand their point of view and acknowledge their feelings. For instance, when addressing medication non-adherence, I might ask, "What challenges are you experiencing with taking your medication?" This allows me to understand the underlying reasons before offering solutions. I focus on collaborative problem-solving, working together to find mutually agreeable solutions.
To resolve conflicts with colleagues, I follow a similar approach. I listen carefully to their concerns, validate their feelings, and express my own perspective clearly and respectfully. I strive to find common ground and work towards a resolution that benefits everyone involved. If necessary, I'm willing to compromise to reach a mutually satisfactory outcome. Documenting the conversation and any agreed upon action items is key to ensure accountability and maintain transparency.
13. Can you discuss your involvement in quality improvement initiatives or research projects in the pharmacy setting?
During my time at [Pharmacy Name], I actively participated in a quality improvement initiative focused on reducing medication errors during dispensing. This involved analyzing incident reports, identifying root causes through fishbone diagrams, and implementing changes to the dispensing workflow, such as double-checking high-risk medications and standardizing label placement. We saw a 15% reduction in reported dispensing errors after implementing these changes.
I also contributed to a research project investigating the impact of pharmacist-led medication reconciliation on hospital readmission rates. My role included collecting patient data, performing medication reviews, and documenting interventions. While the final results are still pending publication, preliminary findings suggest a positive correlation between medication reconciliation and reduced readmission rates, particularly in elderly patients with multiple comorbidities.
14. How do you handle situations where you disagree with a prescriber's medication order?
If I disagree with a prescriber's medication order, my first step is to respectfully and privately discuss my concerns with the prescriber. I would clearly articulate the reasons for my disagreement, backing up my rationale with evidence-based information, such as relevant guidelines, literature, or patient-specific factors like allergies or lab results. I would remain professional and focus on ensuring the best possible outcome for the patient.
If, after the discussion, the prescriber maintains their original order and I still have significant concerns about patient safety, I would then escalate the issue through the appropriate channels, as outlined by institutional policy. This might involve consulting with a more senior pharmacist or the pharmacy director, documenting all communications and decisions thoroughly. My priority is always patient well-being, and I am obligated to act in their best interest even when it requires navigating challenging situations.
15. Explain your experience with sterile compounding and your understanding of USP <797> standards.
I have experience in sterile compounding, primarily in [mention specific settings, e.g., hospital pharmacy, compounding pharmacy]. My experience includes preparing IV medications, including antibiotics, chemotherapy drugs, and total parenteral nutrition (TPN), following strict aseptic techniques. I am proficient in using equipment like laminar airflow workbenches (LAFWs) and biological safety cabinets (BSCs) and performing regular cleaning and maintenance.
I possess a strong understanding of USP <797> standards, including requirements for personnel training and competency, proper garbing and hand hygiene, environmental monitoring (e.g., air and surface sampling), facility design and cleaning, and standard operating procedures (SOPs). I am familiar with immediate-use CSPs, low-, medium-, and high-risk level compounding, and proper documentation practices to ensure compliance and patient safety. I understand the importance of beyond-use dating (BUD) and factors affecting stability.
16. Describe your approach to managing and preventing prescription fraud or abuse.
My approach to managing and preventing prescription fraud or abuse involves a multi-faceted strategy focusing on vigilance, verification, and collaboration. I would first ensure strict adherence to organizational policies and regulatory guidelines related to prescribing practices, controlled substance handling, and patient verification. This includes verifying patient identification, cross-referencing prescription information with patient history to identify potential red flags like unusual quantities or frequent requests from different providers, and utilizing prescription drug monitoring programs (PDMPs) to track controlled substance prescriptions.
Furthermore, I would actively engage in education and training programs for healthcare staff to enhance their awareness of fraud and abuse indicators. This includes recognizing signs of doctor shopping, forged prescriptions, and other suspicious behaviors. I would advocate for the implementation of electronic prescribing systems (e-prescribing) which reduces the risk of altered or forged prescriptions. Regular audits and data analysis would be conducted to identify trends and patterns indicative of potential fraud or abuse, allowing for proactive intervention and corrective action.
17. How do you stay motivated and engaged in your work as a pharmacist, especially during challenging times?
To stay motivated and engaged as a pharmacist, especially during challenging times, I focus on the positive impact I have on patients' lives. Knowing that I'm directly contributing to their health and well-being is a powerful motivator. I also make it a point to continuously learn and expand my knowledge base through journals, conferences, and professional development programs.
Additionally, I find it helpful to set small, achievable goals for each day or week. Celebrating these small wins helps me maintain a sense of accomplishment and momentum. Collaborating with colleagues and actively participating in team discussions also fosters a sense of community and shared purpose, which combats feelings of isolation or burnout during tough periods. Open communication and seeking support when needed are crucial for maintaining motivation and engagement.
18. Discuss your experience with providing clinical pharmacy services, such as medication therapy management or disease state management.
During my experience, I've actively engaged in providing clinical pharmacy services, focusing on optimizing patient outcomes through medication therapy management (MTM). I've conducted comprehensive medication reviews to identify, resolve, and prevent medication-related problems. This involved collaborating with physicians and other healthcare providers to adjust medication regimens based on patient-specific factors, such as comorbidities, lab values, and lifestyle. I also have experience in disease state management, specifically in areas like diabetes and hypertension.
In these settings, I've provided patient education and counseling on medication adherence, proper administration techniques, and potential side effects. I've used tools and resources like patient interviews, electronic health records, and evidence-based guidelines to develop personalized care plans. My goal has always been to improve medication safety, efficacy, and overall patient well-being through a collaborative and patient-centered approach.
19. What strategies do you employ to build rapport and trust with patients?
I prioritize active listening by giving patients my full attention, nodding, and summarizing their concerns to ensure understanding. I use empathetic language, acknowledging their feelings and validating their experiences. Maintaining a calm and professional demeanor while being genuine and approachable helps create a safe space.
Furthermore, I explain procedures and treatment plans clearly and concisely, addressing any questions or anxieties they may have. Transparency regarding potential risks and benefits builds confidence. I respect their autonomy and involve them in decision-making, empowering them to actively participate in their care. Finally, I am mindful of cultural differences and adapt my communication style accordingly.
20. How do you approach continuous learning and professional development to enhance your skills and knowledge as a pharmacist?
To stay current in the pharmacy field, I actively engage in several continuous learning strategies. I regularly read pharmacy journals, attend continuing education (CE) courses and conferences, and participate in online webinars focused on new medications, therapies, and guidelines. I also subscribe to relevant newsletters and follow reputable pharmacy organizations and thought leaders on social media to stay informed about industry trends and emerging best practices.
Furthermore, I actively seek opportunities to expand my knowledge through professional development. This includes pursuing relevant certifications, such as in specialty pharmacy areas, and participating in training programs focused on leadership, communication, and clinical skills. I also proactively seek feedback from colleagues and mentors to identify areas for improvement and tailor my learning accordingly. Finally, I engage in self-directed learning by exploring topics relevant to my practice through online resources and professional networks.
21. Describe your experience in training or mentoring pharmacy students or new pharmacists.
Throughout my career, I've actively sought opportunities to mentor pharmacy students and newly licensed pharmacists. I've guided students during their experiential rotations, providing practical insights into patient counseling, drug information retrieval, and clinical decision-making. I also helped them develop skills in areas like medication therapy management and patient safety.
With new pharmacists, my focus shifts towards navigating the professional landscape. I've offered guidance on career development, including resume building, interview preparation, and exploring specialization options. I've also shared my experiences with ethical considerations and strategies for effective communication with patients and healthcare teams, supporting their transition into independent practice.
22. How do you contribute to a positive and collaborative work environment within the pharmacy team?
I contribute to a positive pharmacy team environment by actively listening to my colleagues, offering assistance whenever possible, and communicating clearly and respectfully. I believe in fostering open dialogue, sharing knowledge, and constructively addressing any conflicts that may arise. I also try to celebrate team successes and acknowledge individual contributions, creating a supportive atmosphere where everyone feels valued and motivated.
Furthermore, I am always willing to learn from others and share my own experiences. I am proactive in maintaining a clean and organized workspace and adhering to established protocols to ensure efficiency and patient safety. I strive to maintain a positive attitude, even under pressure, and contribute to a culture of continuous improvement within the team.
23. Explain your understanding of pharmacoeconomics and how it applies to formulary management and medication selection.
Pharmacoeconomics is the study of the economic value of pharmaceutical products and services. It compares the costs and consequences of different treatment options to determine which provides the best value. This involves assessing factors like drug acquisition costs, administration costs, monitoring costs, and the clinical outcomes achieved, such as improved health, reduced hospitalizations, or increased lifespan.
In formulary management and medication selection, pharmacoeconomics is crucial. Formulary decisions, which drugs are covered, are influenced by cost-effectiveness analyses. Medications demonstrating superior value (better health outcomes per dollar spent) are more likely to be included on the formulary. Pharmacoeconomic data helps healthcare providers and payers make informed choices, balancing clinical efficacy with financial considerations to optimize patient care within budget constraints.
24. Can you discuss your experience with participating in emergency preparedness planning and response in a pharmacy setting?
During my time as a pharmacy intern at [Pharmacy Name], I actively participated in emergency preparedness planning. This involved reviewing and updating the pharmacy's emergency protocols, specifically focusing on scenarios like natural disasters and power outages. I assisted in ensuring adequate stock of essential medications and supplies, and participated in mock drills simulating emergency situations to test our response effectiveness.
I also played a role in responding to a localized water contamination event. My responsibilities included preparing customized hand sanitizers following WHO guidelines, assisting with patient counseling on safe medication handling during the crisis, and coordinating with local health organizations to ensure access to critical medications for affected populations. This experience highlighted the importance of proactive planning and clear communication during emergencies.
Expert Pharmacist interview questions
1. Describe a time you significantly improved pharmacy workflow to enhance patient safety. What metrics did you use to measure success?
During my time at a busy outpatient pharmacy, I noticed a significant bottleneck in the prescription verification process, leading to potential delays and increased risk of errors. To address this, I implemented a barcode-based medication verification system integrated with our existing pharmacy software. This system allowed pharmacists to quickly scan medications during the verification process, automatically comparing the NDC number to the prescription details and patient profile. This reduced the risk of dispensing errors related to wrong drug or wrong dosage.
The success of this intervention was measured by several key metrics. First, we tracked the reduction in dispensing errors per month, observing a 30% decrease in the error rate in the first three months. Second, we monitored the average time spent on prescription verification, which decreased by approximately 15%. Finally, we conducted regular patient satisfaction surveys, which showed an improvement in perceived wait times and confidence in medication safety. By using these metrics, we were able to demonstrate the positive impact of the workflow change on patient safety and pharmacy efficiency.
2. How do you stay current with the latest advancements in pharmacology and therapeutics, and how do you integrate that knowledge into your practice?
I stay current with advancements in pharmacology and therapeutics through a multi-faceted approach. I regularly read leading medical journals such as the New England Journal of Medicine, The Lancet, and JAMA. I also subscribe to pharmacology-specific publications like Pharmacology Research & Perspectives. Attending relevant conferences and workshops, offered by organizations like the American Society for Pharmacology and Experimental Therapeutics (ASPET), is crucial for learning about the latest research directly from experts. Furthermore, I utilize online resources such as PubMed, Medscape, and specialized databases to research specific drugs and therapies.
Integrating this knowledge into my practice involves critically evaluating the evidence presented in these resources. I consider the study design, sample size, and potential biases before accepting the findings. I also participate in continuing medical education (CME) activities to maintain my licensure and expand my expertise. When considering a new treatment option, I discuss the potential benefits and risks with my colleagues, and most importantly, with my patients, to ensure informed decision-making.
3. Explain your approach to managing complex drug interactions, considering both pharmacodynamic and pharmacokinetic factors.
My approach to managing complex drug interactions involves a multi-faceted strategy. First, I thoroughly review the patient's medication list, including over-the-counter drugs and supplements, to identify potential interactions using reliable drug interaction databases and resources like Lexicomp or Micromedex. I consider both pharmacokinetic (PK) and pharmacodynamic (PD) interactions. For PK interactions, I assess how each drug affects the absorption, distribution, metabolism, and excretion (ADME) of other drugs, paying close attention to enzyme inhibition or induction and transporter interactions. For PD interactions, I evaluate the combined effects of drugs on the same physiological systems, such as additive or antagonistic effects on blood pressure or the central nervous system.
Based on the identified risks, I collaborate with the healthcare team to develop a management plan. This might involve selecting alternative medications with a lower interaction potential, adjusting dosages of interacting drugs, spacing administration times, closely monitoring patients for adverse effects, and educating them about potential symptoms to report. I prioritize interventions based on the severity of the potential interaction and the patient's overall clinical status, documenting all recommendations and monitoring plans in the patient's record. Regular reassessment and adjustment of the medication regimen are crucial to ensure patient safety and efficacy.
4. Describe a challenging ethical dilemma you faced in your pharmacy practice and how you resolved it, referencing relevant ethical principles.
In my pharmacy practice, a challenging ethical dilemma arose when a patient, clearly distressed and exhibiting signs of opioid dependence, presented a prescription for a large quantity of oxycodone from an out-of-state physician. My initial reaction was concern about the potential for diversion or misuse, violating the principle of non-maleficence (do no harm).
To resolve this, I first verified the prescription's legitimacy with the physician's office. I then engaged in a private, empathetic conversation with the patient to understand their situation and assess their genuine need for the medication. I also reviewed their prescription history in the state's Prescription Drug Monitoring Program (PDMP). Based on the totality of the information, I collaborated with the physician (after obtaining patient consent) to discuss a possible alternative treatment plan with a lower risk of dependence, while also ensuring the patient received adequate pain management. Ultimately, this approach balanced my duty to prevent harm with the patient's right to appropriate care (beneficence and autonomy).
5. How do you approach developing and implementing new clinical pharmacy services within a healthcare setting?
Developing new clinical pharmacy services requires a systematic approach. First, I'd identify an unmet need or area for improvement by analyzing data, reviewing current practices, and consulting with healthcare providers. This includes understanding the patient population and resource availability. I would then define specific goals and measurable outcomes (e.g., reduced readmission rates, improved medication adherence). A well-defined business plan outlining the service's objectives, implementation strategy, resource allocation, and evaluation methods is crucial. This plan must include necessary training and a timeline for implementation.
Implementation involves piloting the service, collecting data, and adjusting the protocol based on initial findings. Collaboration with relevant stakeholders, such as physicians, nurses, and IT, is essential for successful integration. Continuously monitor key performance indicators, analyze data, and refine the service to optimize its effectiveness and ensure sustainability. This might include presenting findings to a P&T committee to expand the service based on the pilot program results.
6. What strategies do you employ to effectively educate patients with varying health literacy levels about their medications?
To effectively educate patients about their medications, I use a multi-faceted approach tailored to their individual health literacy. I start by assessing their understanding using open-ended questions and observing their body language. Then, I use plain language, avoiding medical jargon, and break down complex information into smaller, manageable chunks. Visual aids like diagrams, pictures, and videos are helpful, as are teach-back methods where the patient explains the information back to me in their own words to confirm comprehension. I also provide written materials that are clear, concise, and at an appropriate reading level and encourage family involvement when appropriate.
I understand that each patient is unique. For some, simplifying the information down to the bare essentials--what the medication is, why they're taking it, how to take it, and potential side effects--is most effective. For others, especially those with higher health literacy, I can provide more detailed explanations and answer more complex questions. I always prioritize building trust and creating a safe space for patients to ask questions and express concerns, regardless of their literacy level. Finally, I ensure my patients leave with resources and contact information for follow-up questions.
7. Explain your experience with formulary management and how you contribute to cost-effective prescribing practices.
My experience with formulary management involves a multifaceted approach to ensure cost-effective prescribing. I've actively participated in Pharmacy and Therapeutics (P&T) committee meetings, contributing to drug evaluations based on clinical evidence, cost analysis, and therapeutic guidelines. I've also assisted in the development and maintenance of formularies, recommending preferred drugs and strategies to optimize medication utilization. This includes analyzing drug utilization data to identify trends, potential overspending, and opportunities for formulary adjustments. I also review and implement prior authorization criteria for non-preferred drugs.
To contribute to cost-effective prescribing, I routinely engage with prescribers to educate them about formulary alternatives, cost-effective prescribing guidelines, and the rationale behind formulary decisions. I also work to educate patients on their medication options and costs. This can involve creating and disseminating educational materials, conducting one-on-one consultations, and participating in pharmacy-led initiatives aimed at promoting adherence and appropriate medication use. I stay informed about new drug approvals, clinical guidelines, and market trends to ensure formulary decisions are based on the most up-to-date information.
8. Describe a time you advocated for a patient's access to medication despite significant barriers. What was the outcome?
During my time as a pharmacy intern, a patient with a complex cardiac condition required a specific anticoagulant that wasn't on the hospital formulary and had a high co-pay. The patient was elderly, on a fixed income, and deeply worried about the cost. I researched alternative medications, but none offered the same efficacy and safety profile for his specific needs. I then contacted the pharmaceutical company directly to explore patient assistance programs. After several calls and completing the required paperwork (which was quite extensive), I secured a temporary supply of the medication at no cost to the patient.
The outcome was positive. The patient received the necessary medication without financial burden, allowing him to continue his treatment uninterrupted. This prevented potential adverse cardiac events. This experience reinforced the importance of persistent advocacy and resourcefulness in ensuring patients have access to the medications they need, regardless of the challenges.
9. How do you handle situations where a physician's prescription appears to be inappropriate or potentially harmful to the patient?
If a physician's prescription seems inappropriate or potentially harmful, my first step is to remain professional and avoid any confrontational behavior. I would discreetly contact the prescribing physician to discuss my concerns. This allows for clarification of the rationale behind the prescription, possible errors in dosage or drug interactions, or any updated patient information I might not be aware of.
If, after speaking with the physician, my concerns remain unresolved, I would consult with a senior pharmacist or the pharmacy manager. They can provide a second opinion and further guidance on how to proceed, ensuring patient safety is the top priority. Depending on the severity of the concern and internal protocols, it may also be necessary to document the interaction and the steps taken to address the potential issue.
10. What is your experience with medication therapy management (MTM) services, and how do you measure the impact of MTM on patient outcomes?
I have experience providing Medication Therapy Management (MTM) services to patients with chronic conditions like diabetes, hypertension, and hyperlipidemia. My responsibilities included conducting comprehensive medication reviews (CMRs), identifying medication-related problems (MRPs), and developing personalized medication action plans in collaboration with patients and their prescribers. I utilized various tools and resources, such as drug interaction databases and clinical guidelines, to optimize medication regimens and improve patient adherence.
To measure the impact of MTM on patient outcomes, I tracked several key performance indicators (KPIs). These included:
- Improved medication adherence rates: measured through prescription refill data and patient self-reporting.
- Reduced medication-related adverse events: monitored through patient feedback and review of medical records.
- Achievement of therapeutic goals: assessed by tracking blood pressure, A1c, and cholesterol levels.
- Cost savings: evaluated by analyzing changes in medication costs and healthcare utilization (e.g., fewer hospitalizations and emergency room visits). I also documented patient satisfaction through surveys and feedback forms. Analyzing these metrics allowed me to demonstrate the value of MTM in improving patient health and reducing healthcare costs.
11. Explain your approach to preventing medication errors and adverse drug events in a high-pressure pharmacy environment.
In a high-pressure pharmacy environment, preventing medication errors and adverse drug events requires a multi-faceted approach. I prioritize verifying each prescription thoroughly, paying close attention to the drug name, dosage, frequency, route of administration, and patient-specific factors like allergies and renal function. I use available technology, such as barcode scanning and automated dispensing systems, to minimize manual entry errors and ensure accurate drug selection.
Communication is also crucial. I proactively clarify any ambiguities with the prescriber and counsel patients on their medications, emphasizing proper administration, potential side effects, and drug interactions. I actively participate in quality improvement initiatives, reporting near misses and contributing to process improvements that enhance patient safety.
12. How do you build and maintain strong collaborative relationships with other healthcare professionals, such as physicians and nurses?
Building strong collaborative relationships in healthcare requires consistent effort and clear communication. I prioritize active listening to understand their perspectives and challenges. Openly sharing information, proactively seeking input, and being responsive to requests helps build trust and mutual respect. I also make it a point to acknowledge their expertise and contributions.
Maintaining these relationships involves consistent communication, regular check-ins (even brief ones), and a willingness to adapt my approach based on their needs. I also focus on conflict resolution with empathy and a focus on finding solutions that benefit both parties and, most importantly, the patient. Participating in interdisciplinary meetings and continuing education also helps foster a sense of shared purpose and understanding.
13. Describe your experience with implementing and managing pharmacy automation technologies, such as dispensing robots or computerized order entry systems.
I have experience with implementing and managing several pharmacy automation technologies. Specifically, I was involved in the deployment and maintenance of a ScriptPro dispensing robot at a high-volume retail pharmacy. My responsibilities included calibrating the robot, troubleshooting mechanical and software issues, and ensuring accurate medication dispensing. I also managed the integration of the robot with our existing pharmacy management system, which involved working with IT to resolve data mapping and communication errors.
Furthermore, I have extensive experience using and maintaining computerized physician order entry (CPOE) systems, such as Epic and Cerner. I was responsible for training pharmacy staff on the proper use of the systems, monitoring order queues for potential errors, and collaborating with physicians and nurses to resolve discrepancies in medication orders. This involved creating and maintaining order sets to improve workflow and reduce medication errors. I have hands-on experience in performing regular system maintenance, troubleshooting errors, and working with the IT department.
14. What is your understanding of pharmacogenomics, and how can it be applied to personalize medication therapy for patients?
Pharmacogenomics is the study of how genes affect a person's response to drugs. It combines pharmacology (the study of drugs) and genomics (the study of genes and their functions) to understand how an individual's genetic makeup influences their reaction to medications.
Pharmacogenomics can personalize medication therapy by identifying genetic variations that affect drug metabolism, efficacy, and toxicity. For example, variations in genes encoding drug-metabolizing enzymes (like CYP2C19 or CYP2D6) can alter how quickly a drug is processed, leading to altered drug levels and effects. By genotyping patients for these variants, clinicians can select the most appropriate drug and dosage for each individual, maximizing therapeutic benefit and minimizing adverse drug reactions. This approach can optimize treatment outcomes and reduce healthcare costs.
15. How do you approach managing and mitigating risks associated with controlled substances in a pharmacy setting?
Managing risks associated with controlled substances in a pharmacy involves a multi-faceted approach. First, strict inventory control is crucial, including regular audits, perpetual inventory systems, and secure storage. Discrepancies must be immediately investigated and documented. Secondly, adherence to legal and regulatory requirements is paramount, including accurate record-keeping, proper prescribing practices, and reporting suspicious activities. Employee training is vital to ensure compliance and prevent diversion.
Mitigation strategies include implementing robust security measures like surveillance systems, restricted access, and alarm systems. Background checks for employees are essential. Developing and enforcing clear policies and procedures regarding controlled substance handling, dispensing, and disposal helps to minimize errors and prevent diversion. Furthermore, fostering a culture of open communication and encouraging employees to report concerns without fear of reprisal is important.
16. Describe your experience with conducting or participating in pharmacy-related research projects or quality improvement initiatives.
During my pharmacy residency, I actively participated in a quality improvement initiative focused on reducing medication errors in the inpatient setting. This involved analyzing medication error reports, identifying common contributing factors, and implementing interventions such as standardizing medication order sets and providing targeted education to nurses and pharmacists. I was responsible for data collection, analysis using statistical software, and presenting findings to the pharmacy and therapeutics committee. We saw a 15% reduction in reported medication errors after implementing the changes.
Furthermore, I assisted with a research project investigating the effectiveness of pharmacist-led medication reconciliation in reducing hospital readmissions. My responsibilities included patient recruitment, obtaining informed consent, performing medication reconciliation interviews, and documenting medication histories. The project provided valuable insights into the role of pharmacists in improving patient outcomes and reducing healthcare costs.
17. How do you handle situations where you encounter conflicting information or guidelines regarding medication use?
When faced with conflicting information or guidelines about medication use, my priority is patient safety. I would first consult established, reputable sources like the official drug monograph (package insert), current clinical practice guidelines from organizations like the FDA or relevant medical societies, and evidence-based databases (e.g., UpToDate, Lexicomp).
If the conflict remains unresolved, I would immediately consult with a senior colleague, a pharmacist, or the prescribing physician. Documenting all sources and the resolution process is crucial for accountability and future reference. Ultimately, the decision must prioritize the patient's well-being based on the best available evidence and clinical judgment.
18. Explain your approach to counseling patients on the safe and effective use of high-risk medications, such as anticoagulants or opioids.
My approach to counseling patients on high-risk medications like anticoagulants or opioids centers on ensuring patient understanding and adherence to minimize potential harm. First, I would assess the patient's current knowledge and any concerns they might have about the medication. I would then explain the medication's purpose, potential benefits, and, most importantly, the significant risks and side effects in plain language, avoiding medical jargon. I would then provide detailed instructions on proper dosage, administration, storage, and what to do if a dose is missed.
For anticoagulants, I emphasize the importance of regular blood monitoring, potential drug and food interactions (like Vitamin K), and signs of bleeding. For opioids, I discuss the risk of dependence, respiratory depression, constipation, and safe disposal methods. I also educate patients about potential interactions with alcohol and other medications. I always encourage patients to ask questions and provide them with written materials or access to reliable online resources to reinforce the counseling session. My goal is to empower patients to actively participate in their own safety.
19. Describe your experience with managing inventory and preventing drug shortages in a pharmacy setting.
In my previous role at [Pharmacy Name], I was responsible for daily inventory management, ensuring adequate stock levels while minimizing waste. I used [Pharmacy System Name] to track inventory, monitor expiration dates, and generate reports to identify slow-moving or overstocked items. I implemented a 'first-expired, first-out' (FEFO) system to reduce drug wastage. Furthermore, I actively monitored wholesaler communications and industry alerts regarding potential drug shortages.
When anticipating or experiencing a shortage, I proactively contacted physicians to suggest alternative medications, communicated with patients about potential delays or alternative options, and explored secondary suppliers to secure necessary medications. I also collaborated with other pharmacies in the area to borrow or share medications in emergency situations, always adhering to legal and ethical guidelines. Regularly reviewing PAR levels based on usage trends and historical data helped to optimize stock and reduce the risk of shortages.
20. How do you stay informed about changes in pharmacy laws and regulations, and how do you ensure compliance with these requirements?
I stay informed about changes in pharmacy laws and regulations through several avenues. I regularly review updates from the state board of pharmacy, the FDA, and professional organizations like the American Pharmacists Association (APhA). Subscribing to newsletters, attending continuing education courses, and participating in webinars are also crucial for staying current.
To ensure compliance, I meticulously document all regulatory changes and update standard operating procedures (SOPs) accordingly. I also conduct regular self-audits to identify any potential gaps in compliance and implement corrective actions. When unsure, I consult with experienced colleagues or legal counsel specializing in pharmacy law.
21. Explain how you would approach implementing a new pharmacy service or program, considering factors such as staff training, resource allocation, and marketing.
To implement a new pharmacy service or program, I'd start with a thorough needs assessment and feasibility study to identify target patients, potential benefits, and resource requirements. Then, I'd develop a detailed implementation plan encompassing staff training (including service-specific knowledge, communication skills, and workflow integration), resource allocation (budget, equipment, space, and personnel), and marketing strategies (awareness campaigns, patient education materials, and referral pathways). Key considerations include securing stakeholder buy-in (pharmacists, technicians, and management) and establishing clear metrics for monitoring program effectiveness and making necessary adjustments.
Ongoing evaluation is crucial. This involves tracking key performance indicators (KPIs) such as patient satisfaction, service utilization rates, and clinical outcomes. Regularly scheduled feedback sessions with staff and patients would help identify areas for improvement and ensure the program remains aligned with evolving patient needs and pharmacy goals. Adapting the service based on data-driven insights is vital for long-term sustainability and success.
22. Describe a time when you had to make a difficult decision regarding patient care or pharmacy operations. What factors did you consider?
During a period of short staffing, we had a surge in antibiotic orders coupled with a critical shortage of IV diluent. Prioritizing immediate patient needs became crucial. The difficult decision was whether to delay preparing some non-urgent antibiotic infusions to conserve diluent for stat orders and critical patients. Factors considered included: 1) Patient acuity and the urgency of antibiotic administration (sepsis vs. prophylaxis); 2) Availability of alternative routes of administration (oral vs. IV); 3) Potential impact of delay on patient outcomes, weighing the risk of delayed treatment against the risk of running out of diluent for more critical cases; and 4) Consultation with physicians to determine the clinical impact of a short delay.
Ultimately, we decided to proceed with the stat orders, contacted physicians about oral alternatives for eligible patients, and temporarily delayed the lowest-priority infusions. We also contacted other hospitals to explore transferring medications from them. This decision, while stressful, ensured that the most critical patients received immediate treatment while mitigating the potential harm of a widespread shortage.
23. How do you handle situations where a patient is dissatisfied with the pharmacy services they have received?
When a patient expresses dissatisfaction, my priority is to actively listen and acknowledge their concerns without interruption. I would then empathize with their situation and try to understand the root cause of their dissatisfaction. Next, I would apologize for the negative experience they had. I would then focus on finding a solution to resolve the issue. This might involve correcting a mistake, offering a refund (if appropriate and within policy), or finding an alternative medication, in consultation with the pharmacist and patient's doctor. Finally, I would follow up to ensure the patient's satisfaction with the resolution and document the complaint and resolution steps for future reference and quality improvement.
24. Explain your approach to mentoring or training pharmacy students or new pharmacists.
My approach to mentoring pharmacy students or new pharmacists centers on fostering a supportive and engaging learning environment. I start by understanding their individual learning styles, strengths, and areas for development. Then, I tailor my mentorship to their specific needs, whether it involves clarifying complex pharmaceutical concepts, guiding them through clinical case studies, or providing feedback on their communication skills. I encourage active participation by asking open-ended questions and promoting critical thinking.
Furthermore, I emphasize the importance of continuous learning and professional development. I share my own experiences and insights, offer resources for further study, and help them build a professional network. I strive to be a role model, demonstrating ethical practice, effective teamwork, and a commitment to patient care. Regular check-ins and open communication are crucial for ensuring that they feel supported and are making progress towards their goals.
25. Describe your experience with using data analytics to identify trends and improve pharmacy performance.
In my previous role at [Previous Company Name], I utilized data analytics to identify key trends impacting pharmacy performance. I primarily used SQL and Excel to extract and analyze data from our pharmacy management system, focusing on metrics like prescription fill rates, inventory turnover, and patient adherence. Through this analysis, I identified several areas for improvement. For example, I discovered a trend of delayed refills for patients on chronic medications due to an inefficient refill reminder system.
To address this, I collaborated with the IT team to implement an automated text message reminder system. This resulted in a 15% increase in on-time refills and improved patient adherence, directly contributing to increased revenue and improved patient outcomes. Additionally, I analyzed inventory data to identify slow-moving items and optimized our ordering process, reducing waste and freeing up valuable shelf space.
26. How do you balance the need to provide efficient pharmacy services with the need to ensure patient safety and quality of care?
Balancing efficiency with patient safety in pharmacy requires a multi-faceted approach. We must use technology effectively such as automated dispensing systems and robust pharmacy information systems that provide decision support and flagging of potential drug interactions or allergies, allowing pharmacists to focus on clinical review and patient counseling. Simultaneously, standardized workflows and regular staff training programs are crucial to minimize errors and ensure adherence to best practices. Continuous monitoring of key performance indicators (KPIs), including dispensing accuracy and patient satisfaction, helps identify areas for improvement. Finally, encouraging a culture of open communication and error reporting without blame ensures that problems are addressed proactively and prevent recurrence.
Patient consultation is key; we need to spend sufficient time with each patient (or caregiver) to explain the medication regimen, potential side effects, and proper administration techniques. This improves patient understanding, adherence and overall safety. Regular audits of dispensing processes and medication storage, combined with feedback from patients and other healthcare professionals, also helps ensure we're maintaining a high quality of care, and proactively addressing any safety concerns.
27. Imagine a new drug has just been approved. How would you prepare the pharmacy staff for dispensing and counseling patients on this medication, considering its unique properties and potential side effects?
First, I'd develop a comprehensive training program. This would include: a thorough review of the drug's mechanism of action, indications, contraindications, dosage, administration, potential drug interactions, and, most importantly, its unique side effect profile. I'd create detailed patient counseling points, emphasizing proper usage and what to watch out for. We'd use resources like the FDA label, manufacturer's information, and relevant clinical guidelines.
Second, I'd implement a system for efficient dispensing and patient education. This involves creating standardized dispensing procedures, developing patient education materials (e.g., leaflets, videos), and incorporating the new drug into our pharmacy software system for accurate record-keeping and drug interaction checks. I'd also organize a Q&A session for staff to address concerns and reinforce their understanding, and implement a way to assess their comprehension before the drug is dispensed.
Pharmacist MCQ
A patient stabilized on warfarin 5mg daily has a CYP2C9 *2/*3 genotype identified. Which of the following is the MOST appropriate initial warfarin dose adjustment?
Options:
A 68-year-old male with a history of hypertension and heart failure is being managed with lisinopril 20mg daily. His recent lab results show a potassium level of 5.8 mEq/L (normal range: 3.5-5.0 mEq/L). Which of the following medications, if started concurrently with lisinopril, would MOST likely contribute to his hyperkalemia?
Options:
A 68-year-old male with hyperlipidemia is stabilized on simvastatin 40 mg daily. His physician prescribes clarithromycin for a respiratory infection. Which of the following is the MOST appropriate recommendation regarding the simvastatin therapy?
options:
Which of the following medications is LEAST likely to cause drug-induced lupus erythematosus (DILE)?
options:
A 68-year-old male has been taking amiodarone for atrial fibrillation for the past year. He presents to his physician complaining of new onset shortness of breath and a dry cough. Which of the following adverse effects of amiodarone is most likely responsible for these symptoms?
Options:
Which of the following is a common adverse effect associated with thiazide diuretics?
A 68-year-old female has been taking omeprazole 20mg daily for the past 5 years for chronic acid reflux. Which of the following is a potential long-term adverse effect associated with prolonged use of proton pump inhibitors (PPIs)? options:
A 62-year-old male with bipolar disorder has been taking lithium for 10 years. He presents to the emergency department with tremors, confusion, and nausea. His lithium level is 2.0 mEq/L (therapeutic range: 0.6-1.2 mEq/L). Which of the following is the MOST appropriate initial management strategy?
options:
A 68-year-old female has been taking prednisone 20mg daily for the past 6 months to manage rheumatoid arthritis. Which of the following adverse effects is she MOST likely to experience due to long-term glucocorticoid use?
options:
A 62-year-old male with type 2 diabetes mellitus has been taking metformin for the past 5 years. He presents to the clinic complaining of fatigue, shortness of breath, and a rapid heart rate. Blood tests reveal a significantly elevated serum lactate level. Which of the following adverse effects of metformin is most likely contributing to this patient's presentation?
A 68-year-old patient with chronic obstructive pulmonary disease (COPD) has been using inhaled fluticasone/salmeterol (Advair Diskus) 500/50 mcg twice daily for the past 5 years. Which of the following is the most likely adverse effect associated with long-term use of inhaled corticosteroids?
A 68-year-old male with chronic osteoarthritis has been taking ibuprofen 600mg three times daily for the past 5 years. Which of the following adverse effects is he MOST at risk for?
A 72-year-old female has been taking alendronate 70 mg weekly for the past 5 years for osteoporosis. Which of the following is a potential adverse effect associated with long-term bisphosphonate use that the pharmacist should monitor for?
Which of the following is a common adverse effect associated with the chronic use of Selective Serotonin Reuptake Inhibitors (SSRIs)?
A patient taking furosemide for heart failure is experiencing muscle weakness and cramps. Which of the following electrolyte imbalances is the most likely cause of these symptoms?
A 55-year-old male with a history of schizophrenia has been taking an atypical antipsychotic medication for the past 10 years. Which of the following is the most likely long-term adverse effect associated with chronic use of atypical antipsychotics?
A 68-year-old male has been taking opioid medications for chronic back pain for the past three years. Which of the following is a common adverse effect associated with long-term opioid use?
A 72-year-old male is started on oxybutynin for urinary incontinence. Which of the following is the most likely adverse effect he will experience?
A 55-year-old patient with a history of asthma has been using an inhaled beta-2 agonist (albuterol) as needed for several years. Which of the following is the most likely adverse effect associated with chronic, excessive use of this medication?
A 72-year-old male with a history of Parkinson's disease has been taking levodopa/carbidopa for the past 5 years. He reports experiencing involuntary, jerky movements, especially affecting his face and limbs, that are interfering with his daily activities. Which of the following is the MOST likely cause of these movements?
options:
A 68-year-old male has been taking oral prednisone 20mg daily for the past 3 years to manage his rheumatoid arthritis. Which of the following adverse effects is he MOST likely to experience as a result of long-term corticosteroid use?
options:
A 25-year-old female presents to her physician complaining of discolored teeth. She reports taking a medication chronically since she was a child. Which of the following medications is MOST likely responsible for this adverse effect?
options:
A patient taking a non-selective Monoamine Oxidase Inhibitor (MAOI) like phenelzine should be educated about potential drug-food interactions. Consumption of foods high in tyramine while on this medication poses a significant risk for which of the following adverse effects?
A 30-year-old female presents to the emergency department after intentionally ingesting 15 grams of acetaminophen approximately 3 hours prior to arrival. Which of the following is the MOST appropriate initial management strategy?
A patient taking digoxin is started on quinidine for atrial fibrillation. Which of the following is the most likely consequence of this drug interaction?
Which Pharmacist skills should you evaluate during the interview phase?
An interview can't reveal everything about a candidate, but it's the perfect time to assess core skills. For pharmacists, certain skills are more important than others. Here’s what to look for.
Pharmaceutical Knowledge
Gauge a candidate's grip on pharmaceutical knowledge with a skill assessment. Adaface offers relevant MCQs to filter candidates effectively.
Let's see how the interviewee will react in a situation where pharmaceutical knowledge is tested. Here is one such interview question.
A patient who is on warfarin is prescribed erythromycin by a doctor for some infection. What is your action and why?
Look for an answer that highlights the understanding of drug interactions between warfarin and erythromycin. A good response would include a suggestion to inform the prescribing doctor of the potential interaction.
Attention to Detail
Screen for attention to detail using targeted assessments. Adaface's Attention to Detail test can help you identify candidates who excel in this area.
Attention to detail is best assessed by posing a question where the candidate needs to apply their attention to identify the right medicine. Here is an interview question.
A prescription reads 'Amoxacillin 250mg q8h'. What additional information would you seek before dispensing this medication?
The ideal candidate will ask for details like patient age, weight, and any known allergies. They should also clarify the route of administration and the duration of treatment.
Communication Skills
Test for effective communication skills with targeted MCQs. Adaface can help you identify candidates who can clearly convey information.
Effective communication is key, so let's see how they communicate medication instructions. Here’s an interview question.
How would you explain to an elderly patient with limited health literacy how to take their new medication, a diuretic, and why it's important?
Look for a candidate who uses simple, clear language and avoids medical jargon. The candidate should demonstrate empathy and confirm the patient's understanding before concluding the explanation.
3 Tips for Using Pharmacist Interview Questions
Before you start putting what you've learned into practice, here are a few tips to help you make the most of your pharmacist interviews. These suggestions will help you streamline the hiring process and ensure you find the best candidate for your team.
1. Leverage Skills Assessments to Refine Your Candidate Pool
Skills assessments can be a game-changer in the early stages of your hiring process. By using them, you gain objective insights into a candidate's abilities, ensuring you're focusing on those who truly possess the skills needed for the role.
For pharmacist roles, consider using assessments to evaluate key areas. For example, the Pharmacist Test assesses core pharmaceutical knowledge, while our test library has cognitive ability tests that measure critical thinking, problem-solving, and attention to detail. These are all important in a pharmacist.
Implementing skills assessments before interviews helps you prioritize candidates with proven abilities. You can also refine your interview questions based on assessment results, diving deeper into specific areas of strength or weakness. Now onto the next tip!
2. Outline Relevant Interview Questions
Time is of the essence during interviews, so carefully selecting the right questions is key. By focusing on the most relevant inquiries, you maximize your chances of evaluating candidates on aspects such as their clinical knowledge, patient counseling skills, and ethical judgment.
Remember to leverage other questions we have from our interview library. For instance, asking about communication skills or cultural fit can provide valuable insights beyond technical expertise. Think about it.
Strategically compiling a targeted set of interview questions ensures you efficiently assess a candidate's most areas without wasting time on redundant topics.
3. Ask Thoughtful Follow-Up Questions
Using the interview questions alone won't always reveal the full picture of a candidate's capabilities. Asking insightful follow-up questions is often a way to gauge the true depth of their understanding and determine whether they can genuinely apply their knowledge to real-world scenarios.
For example, after asking a candidate about their experience with a specific medication interaction, a good follow-up question might be: "Can you describe a time when you identified a potential drug interaction and how you addressed it?" This reveals their problem-solving approach and ability to handle such situations in practice.
Evaluate Pharmacist Skills Accurately to Hire Top Talent
If you're looking to hire pharmacists with specific skills, it's important to verify those skills accurately. Using skills tests is the most effective way to do this. Consider using a skills test like the Pharmacist Test or Pharmacy Technician Test to assess candidates.
Once you've used a skills test to identify the best applicants, you can proceed to interviews. To get started with skills testing and streamline your hiring process, sign up on our platform.
Pharmacist Test
Download Pharmacist interview questions template in multiple formats
Pharmacist Interview Questions FAQs
Basic questions often cover education, licensure, customer service experience, and knowledge of medications.
Intermediate questions might explore problem-solving skills, handling prescriptions, and collaboration with healthcare teams.
Advanced questions often assess knowledge of pharmacology, handling complex patient cases, and regulatory compliance.
Tailor your questions to the specific role requirements, actively listen to responses, and assess both technical skills and soft skills.
Focus on technical expertise, communication skills, problem-solving abilities, and commitment to patient care.
Expert questions would focus on specialty pharmacy, drug development, research, or regulatory affairs.

40 min skill tests.
No trick questions.
Accurate shortlisting.
We make it easy for you to find the best candidates in your pipeline with a 40 min skills test.
Try for freeRelated posts
Free resources